Lamotrigine-Valproate Dosing Calculator
Dosing Safety Guide
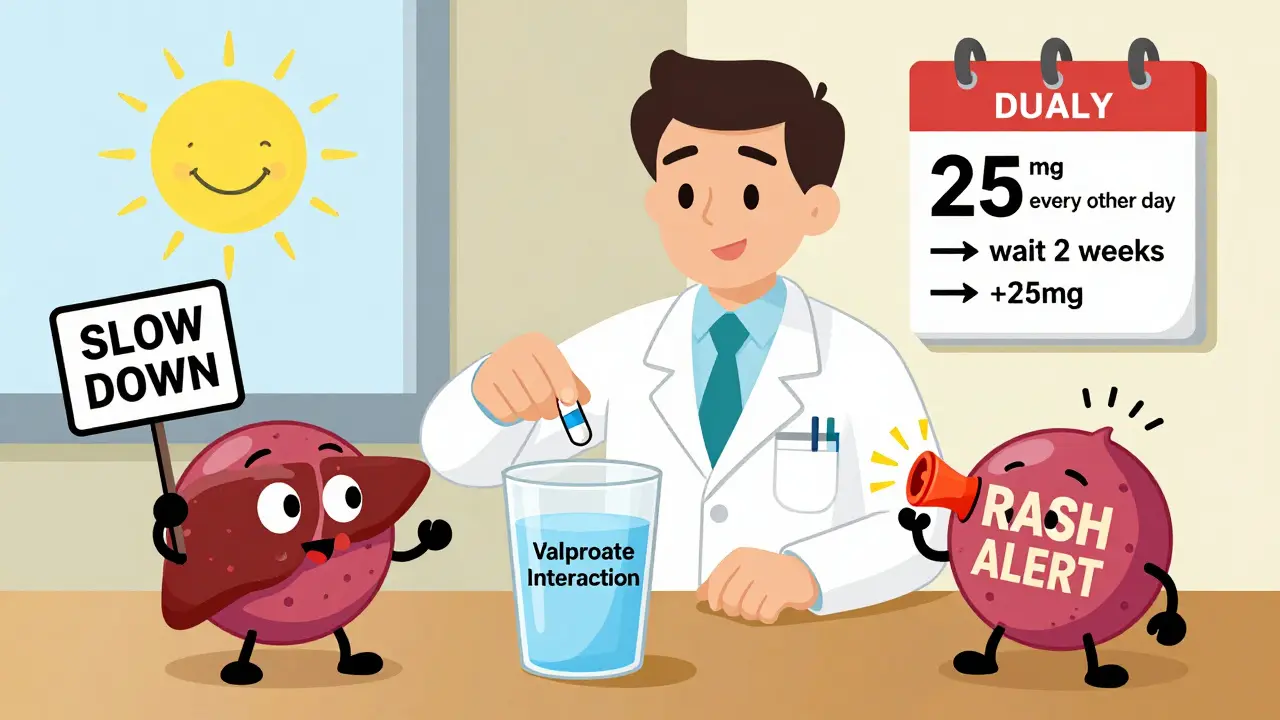
When taking lamotrigine with valproate, your risk of severe rash increases significantly. This calculator helps determine safe dosing based on FDA guidelines and clinical evidence.
Safe Dosing Recommendations
Rash Warning
Stop lamotrigine immediately if you develop any rash, especially if accompanied by fever, mouth sores, or eye irritation. Severe reactions like Stevens-Johnson syndrome can be fatal.
Even mild rashes can progress rapidly. Contact your healthcare provider immediately.
Patient Education
Most rashes appear within the first 8 weeks, especially during dose increases. Children and those with prior antiepileptic rash history are at higher risk.
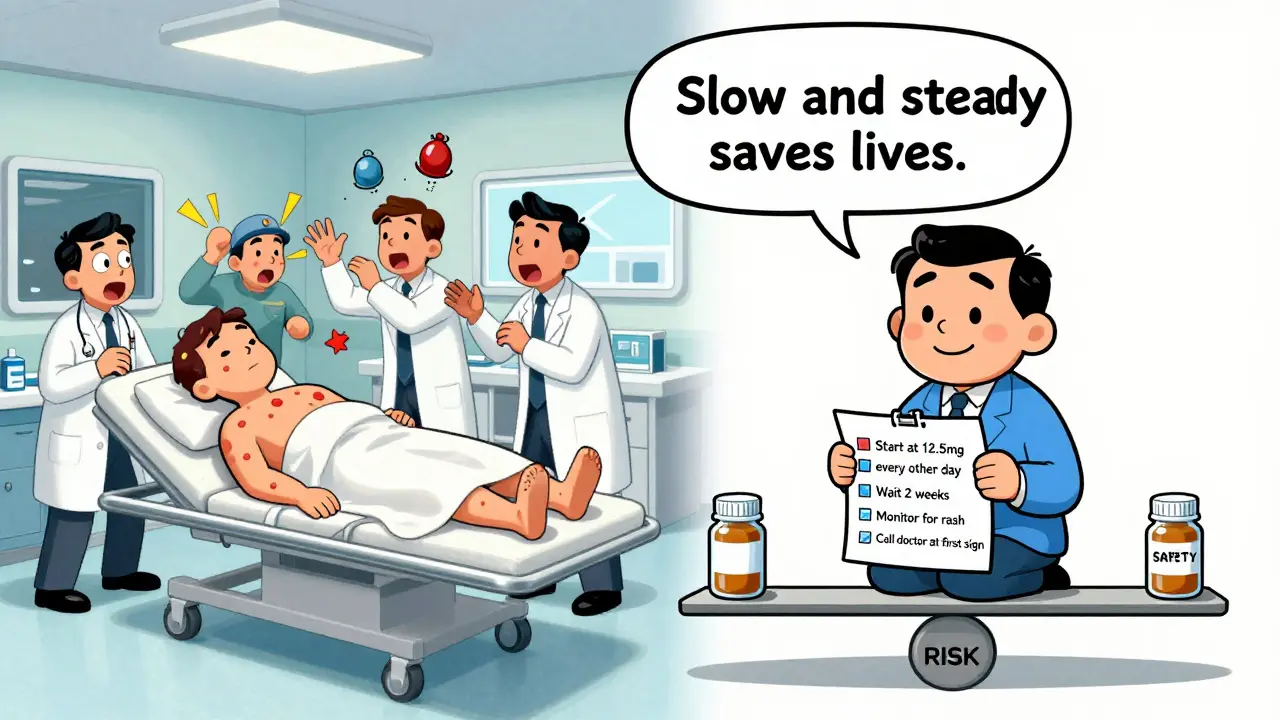
When you’re prescribed lamotrigine and valproate together, it’s not just about treating epilepsy or bipolar disorder-it’s about avoiding a skin reaction that can turn dangerous. This isn’t theoretical. People have ended up in intensive care because their rash turned into Stevens-Johnson syndrome. But here’s the good news: lamotrigine rash risk drops dramatically when you follow the right dosing rules. The science is clear, the guidelines are simple, and the outcome is often preventable-if you know what to do.
Why This Interaction Matters
Lamotrigine and valproate are both widely used. Lamotrigine helps with seizures and mood swings. Valproate works for seizures, migraines, and bipolar disorder. When taken together, they don’t just add up-they change each other’s behavior in your body. Valproate slows down how fast your liver breaks down lamotrigine. That means lamotrigine builds up in your bloodstream faster than normal. And when lamotrigine levels get too high, your risk of a serious skin rash goes up. This isn’t a guess. Studies from the 1990s showed a spike in severe rashes when these two drugs were used together. In 1993, five cases of Stevens-Johnson syndrome were linked to lamotrigine in Germany. By 1999, after doctors started adjusting doses, that number dropped to just three cases-even as more people started taking the drug. The reason? Better dosing.The Science Behind the Risk
Lamotrigine is cleared from your body mainly through glucuronidation. Valproate blocks that process. Studies show this cuts lamotrigine clearance by about half. That’s not a small effect. It means if you take 100 mg of lamotrigine while on valproate, your body treats it like you took 200 mg. Your blood levels double. And higher levels = higher rash risk. The rash isn’t just a mild itch. It can become Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN). These are life-threatening. SJS has a 5-10% death rate. TEN kills up to 35% of people who get it. Most cases happen within the first 8 weeks of starting lamotrigine, especially if you jump straight to a high dose. But even after stopping lamotrigine, symptoms can still show up-like in one 2023 case where an 18-year-old developed a full-body rash and swollen lymph nodes three days after quitting the drug.What Dose Adjustments Actually Look Like
If you’re starting lamotrigine while already on valproate, the standard dosing schedule doesn’t apply. Here’s what works:- Start at 25 mg every other day (not daily). That’s half the usual starting dose.
- Wait two full weeks before increasing.
- Then, increase by 25 mg every two weeks.
- Do not exceed 100 mg per day in the first month.
When to Stop Immediately
A rash is not something to wait out. Even if it looks like a mild sunburn or a few spots, stop lamotrigine the moment you see it. Don’t wait for blisters. Don’t wait for fever. Don’t assume it’s an allergy to something else. In one study of 1,890 patients, the strongest predictor of a drug-related rash was having had one before. If you’ve ever had a rash from another seizure or mood medication, you’re at higher risk. And here’s something many don’t realize: the rash can worsen even after you stop lamotrigine. That’s because the drug stays in your system longer when valproate is slowing its breakdown. So if you notice redness, peeling, or blisters after quitting, call your doctor. You may need steroids or hospital care.Who’s Most at Risk?
Not everyone gets a rash. But some groups are more vulnerable:- Children and teens: Their bodies metabolize drugs differently. FDA warnings specifically mention higher risk in pediatric patients.
- People with prior AED rash: If you had a rash from carbamazepine or phenytoin, your odds jump 3 times.
- Those who rush the dose: Jumping from 25 mg to 100 mg in a week? That’s how you trigger a reaction.
- Patients with autoimmune conditions: While not proven, some case reports suggest a link.
What About Other Drugs?
Lamotrigine doesn’t play well with all antiepileptics. Carbamazepine and phenytoin speed up its metabolism, so you need higher doses. But valproate? It’s the opposite. That’s why switching from one drug to another without adjusting lamotrigine can be dangerous. If you stop valproate, your lamotrigine levels will suddenly drop. You might need to increase your dose to stay stable. But if you start valproate while on lamotrigine, you must cut the lamotrigine dose back. Don’t assume your pharmacist or general doctor knows this. This is specialist-level knowledge. If you’re on both drugs, make sure your neurologist or psychiatrist is managing the interaction-not just prescribing it.Real Cases, Real Lessons
In one 2023 case, an 18-year-old with bipolar disorder developed a full-body rash and swollen lymph nodes after 12 days on lamotrigine and valproate. Her doctors didn’t realize the dose was too high. She had to stop both drugs and get IV steroids. It took weeks to recover. Another patient, a 42-year-old woman, got a mild rash after her doctor increased her lamotrigine too fast. She was on valproate. She stopped the drug, switched to an antihistamine, and recovered in five days. No hospitalization. No long-term damage. She was lucky-because she noticed it early. These aren’t rare. They’re preventable.What to Do Now
If you’re taking both drugs:- Check your current lamotrigine dose. If you started at 50 mg or higher, talk to your doctor about reducing it.
- Ask if your dose was adjusted when valproate was added.
- Review your titration timeline. Were you on 25 mg daily for 7 days? That’s too fast.
- Keep a symptom log. Note any new rash, fever, sore throat, or swollen glands.
- Never stop either drug without medical guidance. Abruptly quitting valproate can cause seizures.
Can you take lamotrigine and valproate together safely?
Yes, but only with careful dose adjustments. Valproate slows down how fast your body clears lamotrigine, which can lead to dangerously high levels. Starting lamotrigine at 25 mg every other day and increasing slowly reduces the risk of severe rash. Always follow your doctor’s titration plan.
How long after starting lamotrigine does a rash usually appear?
Most rashes appear within the first 8 weeks, especially in the first 2-6 weeks. The highest risk is during the initial dose increases. But in rare cases, symptoms can develop even after stopping lamotrigine, because valproate delays its elimination from the body.
What should I do if I notice a rash while on these drugs?
Stop taking lamotrigine immediately and contact your doctor. Do not wait to see if it gets worse. Even a mild rash can progress to a life-threatening condition like Stevens-Johnson syndrome. Avoid taking any other new medications until you’ve been evaluated.
Is lamotrigine rash more common in children?
Yes. The FDA has issued a black box warning for lamotrigine in children and adolescents, especially when used with valproate. Their metabolism and immune response differ from adults, making them more susceptible. Starting doses should be even lower-often 12.5 mg every other day-and titrated more slowly.
Can you switch from valproate to another drug to avoid the interaction?
Yes, if your condition allows it. Alternatives like lithium, carbamazepine, or oxcarbazepine may be considered for mood stabilization. For epilepsy, levetiracetam or topiramate could be options. But switching must be done under close supervision to avoid seizures or mood instability. Never stop valproate abruptly.

Steve DESTIVELLE
February 11, 2026 AT 14:44Valproate doesn't just slow lamotrigine it rewrites the rules of engagement
Every dose increase is a gamble with your skin as the currency
We treat medicine like it's software updates but biology has no undo button
That rash isn't a side effect it's a protest
And if you think you can outsmart metabolism with willpower you're already in the ICU
There's no such thing as safe when the liver is being held hostage
Slow down not because the guidelines say so but because your cells are begging you to
The FDA didn't write those warnings for lawyers they wrote them for people who think they're invincible
And if you're still reading this you're probably the one who needs to hear it
Don't optimize for speed optimize for survival