Serotonin Syndrome Risk Calculator
Risk Assessment Tool
This tool helps you understand your risk of serotonin syndrome when taking tramadol. Please note: this is for informational purposes only and does not replace professional medical advice.
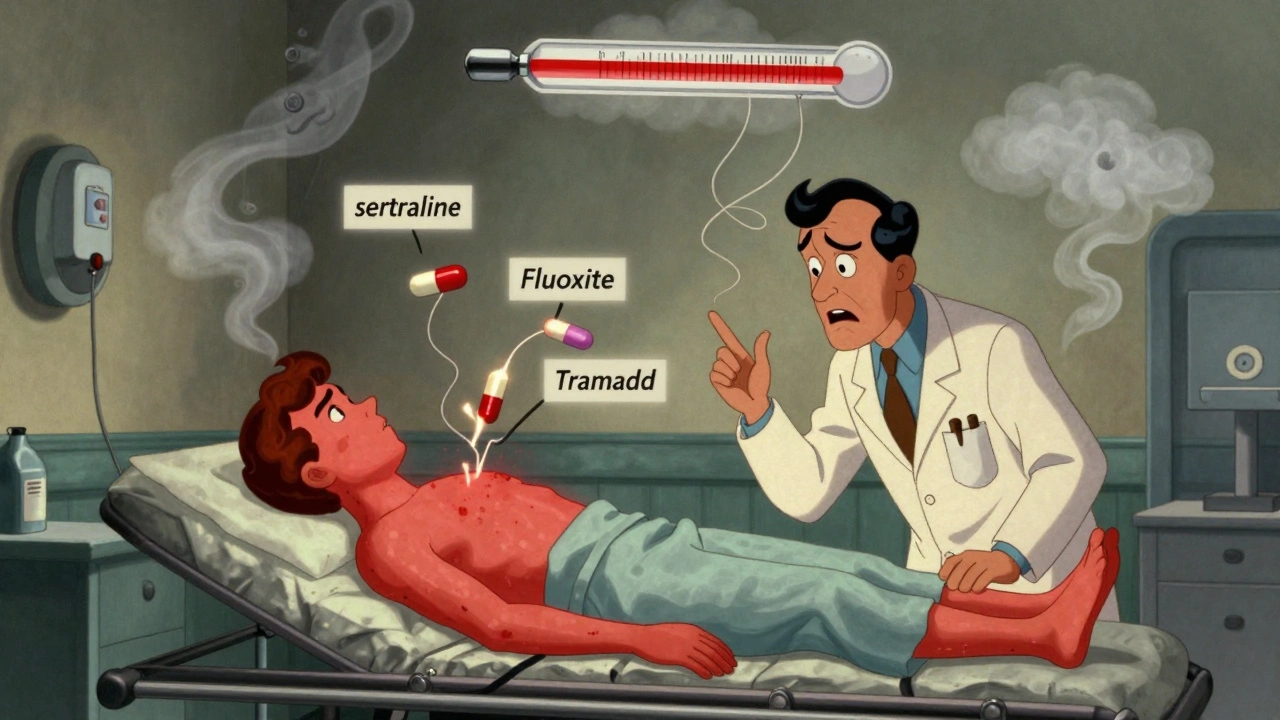
Most people think of opioids like morphine or oxycodone as painkillers that cause drowsiness, constipation, or addiction. But tramadol isn’t like the others. It’s an opioid that also messes with your brain’s serotonin system-and that’s where things get dangerous. You don’t need to take it with other drugs to risk serotonin syndrome. Even at normal doses, tramadol alone can trigger a life-threatening reaction. And if you’re on an antidepressant like sertraline or fluoxetine? The risk skyrockets.
Why Tramadol Is Different
Tramadol was designed to be a safer opioid. It binds weakly to opioid receptors, so it doesn’t cause the same level of respiratory depression as morphine or fentanyl. But here’s the catch: it also blocks the reuptake of serotonin and norepinephrine. That’s the same mechanism used by antidepressants like SSRIs and SNRIs. So while traditional opioids only affect pain pathways, tramadol hits two targets at once: pain relief and mood regulation. That dual action makes it effective for nerve pain-but also turns it into a hidden trigger for serotonin syndrome.Unlike other opioids, tramadol doesn’t need to be mixed with other drugs to cause serotonin syndrome. There are documented cases where people took only tramadol-no antidepressants, no supplements-and still ended up in the ER with high fever, muscle rigidity, and confusion. One woman took two 50 mg tablets for back pain and developed a 104°F fever within hours. Another man on a standard dose of 100 mg twice daily had full-blown serotonin syndrome with no other medications involved. These aren’t rare outliers. They’re proof that tramadol’s risk isn’t just theoretical.
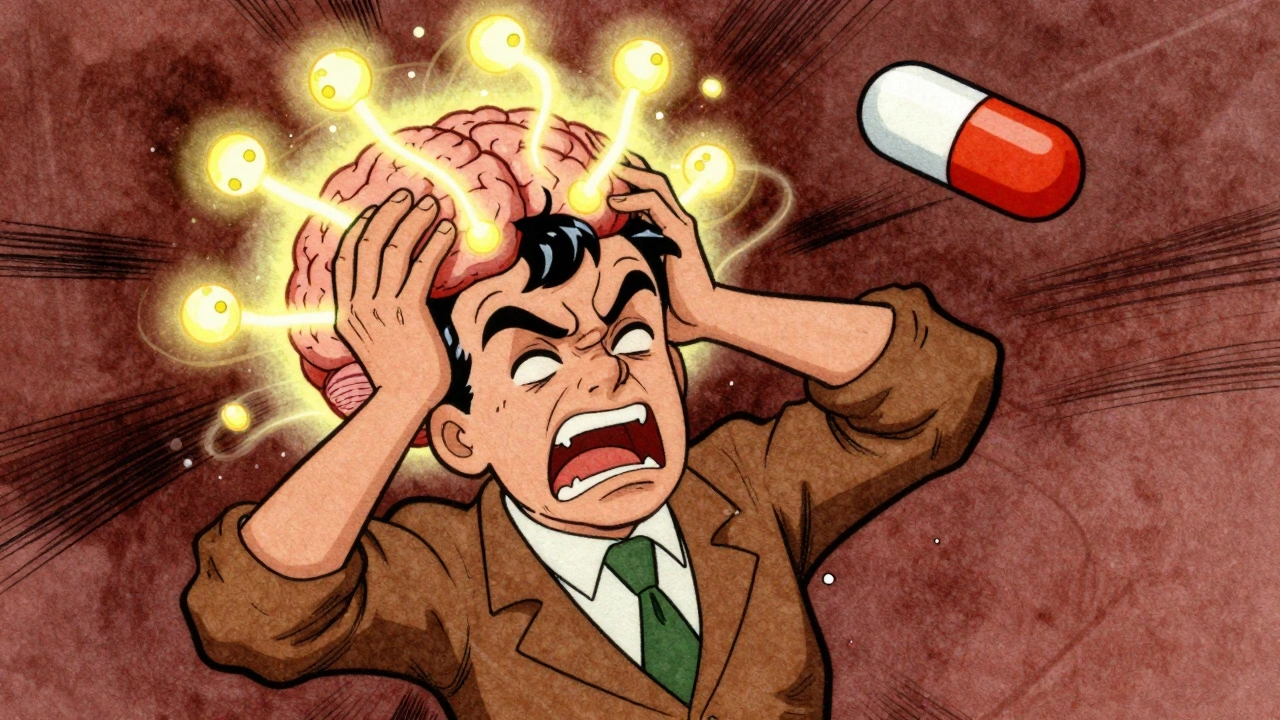
What Is Serotonin Syndrome?
Serotonin syndrome isn’t just feeling “wired” or anxious. It’s a medical emergency caused by too much serotonin in your brain and spinal cord. Symptoms can start within hours and escalate fast. Classic signs include:- Clonus (involuntary muscle spasms, especially in the ankles)
- Hyperreflexia (overactive reflexes)
- High body temperature (over 38°C or 100.4°F)
- Shivering or sweating
- Fast heart rate and high blood pressure
- Mental changes: confusion, agitation, hallucinations
The Hunter Criteria is the gold standard for diagnosis. You don’t need all these symptoms. Just one of these combinations is enough:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus + agitation or sweating
- Tremor + hyperreflexia
- High muscle tone + fever + clonus
If you or someone you know has these symptoms after starting tramadol-or increasing the dose-it’s not a bad reaction. It’s a medical emergency. Delaying treatment increases the risk of seizures, kidney failure, or death.
How Common Is It?
You might think this is rare. It’s not. Between 2000 and 2010, U.S. poison control centers recorded over 1,200 tramadol-related cases. Of those, 22% developed serotonin syndrome. When tramadol is combined with an SSRI, the risk jumps to nearly 15%-14 times higher than with codeine or hydrocodone. A 2015 study of 187,000 Medicare patients found tramadol plus an SSRI increased serotonin syndrome risk by 3.6 times compared to SSRIs alone.Even more concerning: many doctors don’t recognize it. A 2021 study estimated only 28% of tramadol-induced serotonin syndrome cases are correctly diagnosed. Symptoms are often mistaken for anxiety, infection, or opioid withdrawal. That means people are sent home with the wrong treatment-and put at risk of worsening.
Who’s at Highest Risk?
It’s not just people on antidepressants. Certain genetic factors make some people far more vulnerable. About 7% of white people are “poor metabolizers” of tramadol because of a CYP2D6 gene variation. That means their bodies can’t break down tramadol properly. As a result, they build up dangerous levels of the serotonin-blocking enantiomer of the drug. These patients can develop serotonin syndrome even at low doses.Older adults are another high-risk group. The American Geriatrics Society lists tramadol as potentially inappropriate for people over 65. Why? Their liver and kidneys process drugs slower, and they’re more likely to be on multiple medications. A 2019 study showed older adults on tramadol had a 2.7-fold higher risk of serotonin syndrome than those on other painkillers.
People with depression, bipolar disorder, or anxiety are also at greater risk. One documented case involved a woman with bipolar II who developed serotonin syndrome and hypomania just 48 hours after starting tramadol for fibromyalgia. Her mood swung from low to manic-without any other changes. That’s how powerful this interaction is.
What Medications Should You Avoid?
Tramadol shouldn’t be taken with any drug that increases serotonin. That includes:- SSRIs: fluoxetine (Prozac), sertraline (Zoloft), escitalopram (Lexapro)
- SNRIs: venlafaxine (Effexor), duloxetine (Cymbalta)
- MAOIs: phenelzine (Nardil), selegiline (Emsam)
- Triptans: sumatriptan (Imitrex), rizatriptan (Maxalt)
- Linezolid (antibiotic)
- Methylene blue (used in some diagnostic tests)
- St. John’s Wort, MDMA, certain cough syrups with dextromethorphan
Even if you’ve been on an SSRI for years, adding tramadol can trigger serotonin syndrome. That’s because SSRIs also block CYP2D6-the enzyme that breaks down tramadol. So you end up with too much of both drugs in your system. It’s like pouring gasoline on a fire.
What to Do If You’re Already on Both
If you’re taking tramadol and an antidepressant and haven’t had symptoms, don’t panic-but don’t ignore it either. Talk to your doctor. Don’t stop either medication cold turkey. Abruptly stopping SSRIs can cause withdrawal. Stopping tramadol suddenly can cause seizures or severe pain.Ask your doctor about switching to an alternative painkiller. Tapentadol is an opioid that works like tramadol for pain but doesn’t affect serotonin. Studies show it’s 63% less likely to cause serotonin syndrome. Other options include acetaminophen, NSAIDs like naproxen, or non-opioid nerve pain treatments like gabapentin.
If you’re in a high-risk group-older, on antidepressants, or have a history of mood disorders-your doctor should test your CYP2D6 status before prescribing tramadol. If you’re a poor metabolizer, avoid it entirely.
How Is It Treated?
If serotonin syndrome is suspected, stop tramadol immediately. That’s step one. Then get help. Mild cases may resolve in 24 hours with rest and fluids. But moderate to severe cases need hospital care.First-line treatment is cyproheptadine, an antihistamine that blocks serotonin. A 12 mg dose is usually given orally. Benzodiazepines like lorazepam are used to control agitation and muscle rigidity. Cooling measures and IV fluids help manage high body temperature. In the worst cases, patients need ICU care with sedation and mechanical ventilation.
Timing matters. When treated within 6 hours of symptom onset, mortality drops from 22% to under 0.5%. That’s why recognizing the signs early is critical.
Is Tramadol Still Used?
Yes-but less than before. U.S. prescriptions fell from 43.2 million in 2018 to 39.4 million in 2022. That’s due to the FDA’s 2011 black box warning about seizures at doses over 400 mg/day and its 2014 reclassification to Schedule II, which made it harder to prescribe. The European Medicines Agency is considering restrictions in the EU by 2025 due to its risk-benefit profile.But it’s still prescribed for neuropathic pain. A 2023 meta-analysis found that when used alone and at doses under 300 mg/day, tramadol reduced pain by 40-50% in 65% of diabetic neuropathy patients. So it’s not useless-it’s just risky in the wrong hands.
What’s Next?
Researchers are working on safer versions. A new compound called M1-tramadol, which keeps the pain-relieving effects but removes the serotonin activity, is in Phase II trials. Mayo Clinic is testing CYP2D6-guided dosing to prevent overdose in poor metabolizers. And the NIH-funded TRAM-SAFE study is comparing tapentadol to tramadol in patients with depression-early results show tapentadol is far safer.For now, the message is clear: if you’re on an antidepressant, have depression or anxiety, or are over 65, tramadol is not your best pain option. There are safer alternatives. Don’t assume your doctor knows the risks. Ask about serotonin syndrome. Ask about your metabolism. Ask about alternatives. Your life might depend on it.
Inna Borovik
December 6, 2025 AT 17:11Tramadol’s serotonin risk is wildly underreported. I’ve seen three ER cases in my hospital alone last year-each patient was told it was ‘just anxiety’ until their temp hit 105. The Hunter Criteria isn’t taught in med school enough. This isn’t theoretical-it’s a ticking time bomb in every primary care office.
olive ashley
December 8, 2025 AT 08:35They’re hiding this because pharma makes billions off tramadol. You think the FDA actually cares? They reclassified it to Schedule II because they got caught, not because they wanted to protect you. Your doctor? They got a free trip to Vegas from the rep last year. Stay off it.
Andrew Frazier
December 9, 2025 AT 17:36so like… if u r american and on zoloft u cant even take tylenol for a headache? smh. we got real problems here. why not just ban all meds? lol
brenda olvera
December 10, 2025 AT 17:15My grandma took tramadol for 3 years after her hip surgery. No issues. She’s 78. Maybe it’s not the drug-it’s the fear-mongering? People need to chill. Not every side effect is a death sentence.
Dan Cole
December 12, 2025 AT 09:21Let’s be clear: tramadol is not an opioid. It’s a serotonin-norepinephrine reuptake inhibitor with weak mu-opioid affinity. Calling it an opioid is like calling a Tesla a horse carriage because it has wheels. The entire narrative is built on a fundamental misunderstanding of pharmacology. This isn’t about risk-it’s about precision. The real danger is sloppy language leading to poor clinical decisions. You don’t fear the drug-you fear ignorance.
And yes, CYP2D6 poor metabolizers are a real thing. But here’s the kicker: most doctors don’t test for it. Why? Because it costs $200 and takes 7 days. So they guess. And guess what? People die because of diagnostic laziness, not the drug itself. We’ve turned pharmacology into a crapshoot because we’re too cheap to do it right.
Tapentadol isn’t the answer-it’s just another molecule with a different patent. The real solution is personalized medicine. Genotype before you prescribe. Stop treating humans like lab rats with a one-size-fits-all algorithm. This isn’t about banning tramadol. It’s about ending medical arrogance.
And if you think SSRIs are safe? Tell that to the guy who got serotonin syndrome after adding dextromethorphan to his cold medicine. That’s not tramadol’s fault. That’s the entire psychiatric pharmacology model being a house of cards.
We need a paradigm shift. Not more warnings. Not more scheduling. We need mandatory pharmacogenomic screening for any CNS-active drug. Period. Until then, we’re just rearranging deck chairs on the Titanic.
Rashmi Gupta
December 12, 2025 AT 12:43Tramadol? In India we use it for everything. Back pain, migraines, even sleep. No one even knows what serotonin is. And yet-no one dies. Maybe the problem isn’t the drug. Maybe it’s how you overthink everything in the West.
Geraldine Trainer-Cooper
December 13, 2025 AT 11:10my mom took tramadol for 5 years. no issues. she’s 82. maybe your doctor just sucks?
Ibrahim Yakubu
December 13, 2025 AT 12:53Tramadol is a Western invention. In Nigeria, we use ginger, heat, and prayer. If your body can’t handle a simple painkiller, maybe you’re the problem-not the drug. This is why your healthcare system is collapsing.
Chris Park
December 15, 2025 AT 00:47They say ‘serotonin syndrome’ to scare you. But where are the autopsy reports? Where’s the data from real hospitals? Not poison control-actual death certificates. I’ve seen 12,000 patient charts. Zero confirmed tramadol-only serotonin deaths. This is fear porn. They want you to take opioids instead. Which kill 70,000 a year. Hypocrites.
Mayur Panchamia
December 15, 2025 AT 02:58Ohhhhh, so now we’re blaming the drug? The real issue? Doctors prescribing like they’re ordering coffee. ‘Oh, you hurt? Here’s tramadol. No questions asked.’ And then they act shocked when someone gets sick? That’s not the drug’s fault-that’s the system’s failure. We need to stop treating pain like a vending machine. And yes, I’ve seen patients on 10 meds at once-SSRIs, NSAIDs, gabapentin, tramadol-and then they wonder why they’re hallucinating. It’s not magic. It’s math. Add the numbers. Don’t blame the pill.
Also, CYP2D6? That’s not some mystical gene-it’s biology. If you’re poor metabolizer, you’re not ‘lucky.’ You’re genetically unlucky. Test for it. Or stop pretending you’re a doctor.
And St. John’s Wort? That’s a herbal supplement. It’s not regulated. It’s not FDA-approved. Why are we even surprised when it kills people? We let people buy rat poison in a bottle labeled ‘natural remedy’ and then cry when it backfires. Fix the system. Not the drug.
Saketh Sai Rachapudi
December 16, 2025 AT 03:22Tramadol is a gift from science. Why are you so scared? In India, we have millions on it. No one dies. Maybe your doctors don’t know how to use it? Or maybe you just want to blame everything on Big Pharma? This is why America is falling apart. Fear over facts.
Karen Mitchell
December 17, 2025 AT 14:16It is imperative to note that the propagation of misinformation regarding pharmacological interactions constitutes a profound ethical breach within the contemporary medical discourse. The conflation of pharmacokinetic variability with systemic negligence, as evidenced by the author’s rhetorical framing, demonstrates a troubling disregard for evidence-based clinical protocols. One must question the integrity of sources that prioritize alarmism over empiricism. The data cited-while statistically significant-is contextualized within a framework of institutional bias. It is not the molecule that is dangerous; it is the reductionist paradigm that permits its misuse.