Every day, pharmacy technicians handle thousands of prescriptions. Most of them-over 90%-are for generic drugs. But knowing the difference between a brand name and its generic version isn’t just helpful. It’s life-or-death. A mix-up between hydroxyzine and hydralazine, two look-alike, sound-alike drugs, has caused serious harm. One wrong pill can lead to a heart attack, an allergic reaction, or worse. That’s why training pharmacy technicians in generic drug competency isn’t optional-it’s the foundation of safe pharmacy practice.
Why Generic Drug Knowledge Is Non-Negotiable
Generic drugs make up the backbone of modern pharmacy. They’re cheaper, widely available, and just as effective as their brand-name counterparts. But they’re not always easy to identify. The same medication can have dozens of generic versions from different manufacturers, each with a different name, color, or shape. A technician who doesn’t know the difference between glipizide and glyburide-both diabetes drugs but with different dosing and risks-could dispense the wrong one. And that’s not hypothetical. The Institute for Safe Medication Practices reports that 10-15% of medication errors linked to pharmacy technicians involve generic/brand confusion. The stakes are high. In the U.S., medication errors contribute to about 7,000 deaths each year. Generic drug misidentification plays a role in a significant portion of those. That’s why certification bodies like the Pharmacy Technician Certification Board (PTCB) and the Department of Veterans Affairs (VA) now treat generic drug knowledge as a core competency-not a bonus skill.What the Standards Actually Require
If you’re training to become a certified pharmacy technician, you need to know more than just “what’s the generic for Lipitor?” You need to know the full picture. Here’s what the major standards demand:- PTCB Certification (CPhT): As of 2026, 18% of the exam tests your ability to identify generic names, brand names, drug classifications, and therapeutic duplications. You must know at least 200 of the most commonly prescribed medications.
- VA Qualification Standard HT38: Pharmacy technicians working in VA hospitals must recognize 100% of Schedule II-V controlled substances by both brand and generic name. Higher-level technicians are expected to understand regulatory quality standards and complex drug programs.
- ASHP Model Curriculum: Hospital-based technicians must recognize high-alert medications-like insulin, heparin, and warfarin-by generic name and understand their therapeutic class and dosing risks.
- State Requirements: All 50 states require generic drug knowledge for licensure, but the depth varies. California asks for mastery of 180 drugs; Texas only 120. This inconsistency makes it harder for technicians to move between states.
How Training Programs Are Adapting
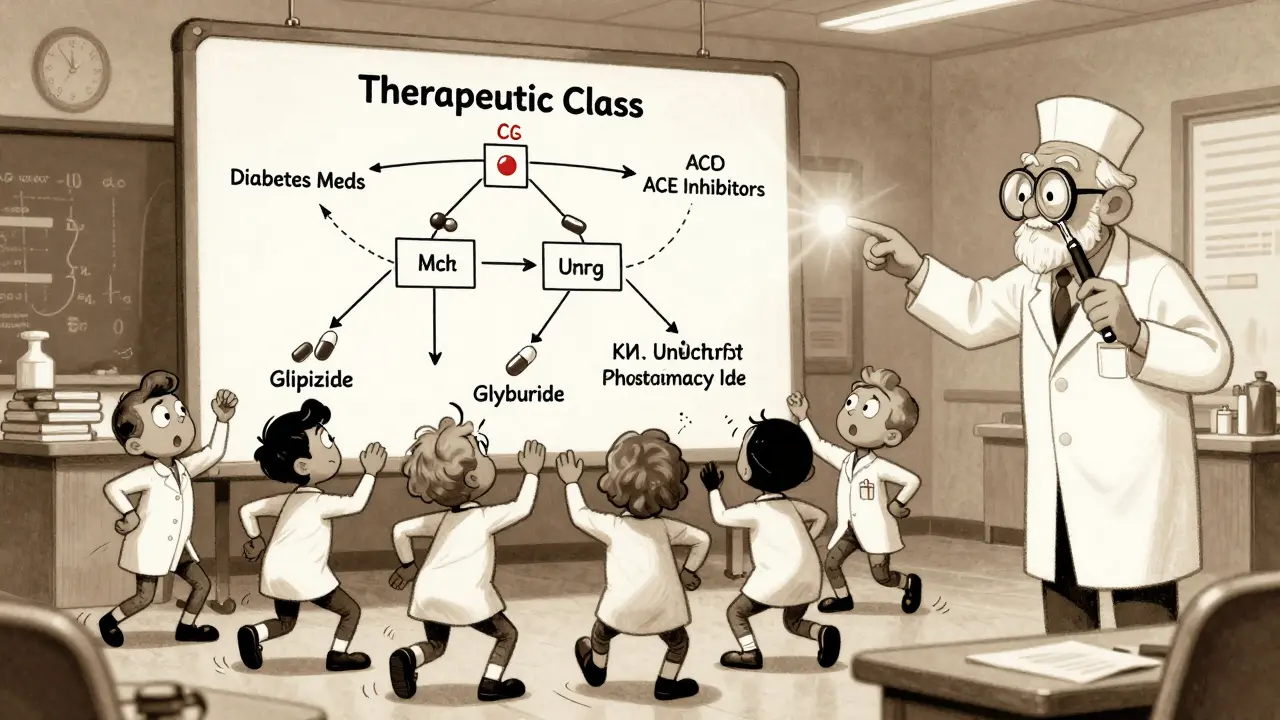
Most pharmacy technician programs now structure their drug knowledge section around the Top 200 Drugs list, which includes the most frequently prescribed medications in the U.S. But memorizing 200 names isn’t enough. The best training programs teach more than rote recall-they teach patterns.- Group by Therapeutic Class: Instead of learning “metformin,” “glimepiride,” and “pioglitazone” as isolated facts, trainees learn they’re all oral diabetes medications. That way, even if a new generic hits the market, they can infer its use.
- Use Visual Cues: Many technicians swear by learning drugs by shape, color, and imprint. A red, oval pill with “50” on one side? That’s likely generic sildenafil. A white, round tablet with “T 10” on it? That’s tenmg of tramadol. Visual learners find this far more effective than flashcards.
- Practice with Real Scenarios: Training shouldn’t be done in a vacuum. Simulated prescription fills, error drills, and barcode scan failures help technicians build confidence under pressure.
The Biggest Challenges Technicians Face
Even with good training, the job gets harder every month. Here’s why:- Constant Change: The FDA approves 15-20 new generic drugs every month. A drug you learned in January might be manufactured by a different company by June-and its appearance changes.
- Look-Alike, Sound-Alike (LASA) Drugs: The ISMP lists 37 high-risk pairs. Examples: clonazepam vs. clonidine, doxepin vs. doxycycline. One letter, one syllable difference. One mistake, potentially fatal.
- Outdated References: Many independent pharmacies still use printed drug guides updated only once a year. That’s dangerous. A 2024 NCPA survey found 43% of community pharmacies rely on these outdated tools.
- Regional Differences: A drug called “Amlodipine Besylate” in New York might be labeled “Norvasc” in Texas, even though they’re the same. Technicians must adapt to local formularies and labeling practices.
What Works: Real Stories from the Front Lines
Pharmacy technicians aren’t just following rules-they’re finding real ways to get better. One technician, who goes by “PharmTech2020” on Reddit, spent eight weeks using flashcards and classification charts to memorize the top 200 drugs. She says her error rate dropped in half within a month. Another, “GenericGuru,” uses the “color-shape-imprint” method and says it works better than memorization for visual learners. In a Pharmacy Times poll, 68% of technicians agreed. A technician from Texas, “Tech4Life,” failed the PTCB exam twice before switching to the RxTechExam Top 100 guide. She focused on drug class, therapeutic use, and common side effects-not just names. She scored 94% on the generic drug section the third time. These aren’t outliers. They’re proof that structured, active learning works.
The Future: Where Generic Competency Is Headed
The standards aren’t static. They’re evolving.- Biosimilars: With 25 biosimilars approved since 2015, training now includes understanding naming conventions like “-mab” for monoclonal antibodies and how biosimilars differ from traditional generics.
- Pharmacogenomics: By 2030, experts predict generic drug training will include genetic markers-like whether a patient metabolizes clopidogrel poorly, making generic versions ineffective.
- Dynamic Assessment: Static lists won’t cut it anymore. The University of North Carolina’s Dr. Karen Smith argues that competency standards must adapt in real time, not annually. Some institutions are testing digital platforms that auto-update drug lists based on FDA announcements.
- Medicare Part D: Starting in 2025, Medicare Part D contractors must verify that pharmacy technicians can correctly identify generic substitutions. This is now a federal compliance issue.
What You Can Do Right Now
Whether you’re a student, a new technician, or a seasoned pro looking to sharpen your skills, here’s how to improve your generic drug competency today:- Download the PTCB Top 200 Drug List (free on their website) and start grouping drugs by class.
- Use a free app like “RxList” or “Epocrates” to check drug appearances and imprint codes daily.
- Practice with a partner: Quiz each other on brand/generic pairs during breaks.
- Ask your manager for access to the pharmacy’s formulary list and compare it to what’s in your training materials.
- Join a community like r/pharmacytech on Reddit. Read the threads. Learn from others’ mistakes.
Why are generic drugs so important for pharmacy technicians to know?
Over 90% of prescriptions filled in the U.S. are for generic drugs. Pharmacy technicians are often the first to verify these medications. If they can’t distinguish between a brand name and its generic version-or confuse similar-sounding generics-they risk dispensing the wrong drug. This contributes to medication errors, which cause thousands of injuries and deaths each year. Knowing generics isn’t just part of the job-it’s a patient safety requirement.
How many generic drugs should a pharmacy technician know?
Most certification programs require knowledge of at least 200 commonly prescribed medications by both generic and brand name. The PTCB exam focuses on the top 200, while the VA requires mastery of 300 high-use drugs, including all controlled substances. Some states, like California, require knowledge of 180 drugs; others, like Texas, require only 120. The goal is to know the drugs you’ll see most often-and be able to recognize high-alert ones like insulin, warfarin, and opioids.
What’s the difference between PTCB and ExCPT certification in terms of generic drug knowledge?
The PTCB exam tests knowledge of about 200 drugs, with 18% of the exam focused on generic/brand identification, drug classification, and therapeutic duplication. The ExCPT from the National Healthcareer Association covers around 150 drugs. This creates a 25% knowledge gap between the two certifications. PTCB is more widely accepted, especially in hospitals and VA facilities, while ExCPT is common in community pharmacies. Most employers prefer PTCB certification due to its broader scope.
How do I study for generic drug identification if I’m a visual learner?
Focus on the physical characteristics of pills: shape, color, and imprint code. Many technicians find that grouping drugs visually-like putting all red oval pills together-helps them recall names faster than flashcards. Apps like Epocrates show images of pills and their imprints. You can also print out pill identification charts and stick them on your workspace. Reddit user “GenericGuru” says this method cut their study time in half and improved recall accuracy.
Are there tools or apps that help pharmacy technicians learn generic drugs?
Yes. Free tools like RxList, Epocrates, and Medscape offer pill identification, drug class breakdowns, and generic/brand name cross-references. The PTCB and RxTechExam offer downloadable Top 200 and Top 100 drug lists with classifications. Some pharmacies use AI-powered training platforms that simulate real dispensing scenarios. The key is to use these tools daily-not just before an exam. Consistent exposure builds automatic recognition.
What happens if a pharmacy technician doesn’t meet generic drug competency standards?
Failure to meet competency standards can lead to higher error rates, disciplinary action, or loss of certification. The PTCB requires passing the certification exam to maintain CPhT status. In hospitals and VA facilities, technicians who score below 90% on quarterly assessments may be required to retake training or be temporarily reassigned. In extreme cases, repeated errors can lead to termination or legal liability. Generic drug knowledge is now tied to accreditation, reimbursement, and patient safety metrics.
Is memorizing drug names enough, or should I understand drug classes too?
Memorizing names is necessary, but not sufficient. Understanding drug classes-like knowing that all “-pril” drugs are ACE inhibitors-lets you reason through unfamiliar generics. If you see a new drug ending in “-statin,” you know it’s a cholesterol-lowering medication, even if you’ve never seen the brand name. Experts like Dr. Jerry Fahrni argue that shifting focus from rote memorization to therapeutic understanding could reduce medication errors by up to 30%. The future of pharmacy tech training is moving toward this approach.

Swapneel Mehta
December 20, 2025 AT 19:15Been working as a tech for 7 years now. The first time I混了 up hydroxyzine and hydralazine, I almost quit. Turns out, I wasn't alone. After that, I started using the color-shape-imprint method religiously. Now I can spot a pill from 10 feet away. It's not magic, just repetition.
Cameron Hoover
December 22, 2025 AT 11:25Let me tell you something that keeps me up at night. The FDA approves 15-20 new generics every month. Meanwhile, my pharmacy still uses a 2021 printed guide. That’s not negligence-that’s a death sentence waiting to happen. Someone needs to burn those books down.
Stacey Smith
December 22, 2025 AT 11:57Anyone who thinks this is just about memorizing names doesn’t understand how the system works. This isn’t a test. This is survival. If you can’t tell the difference between glipizide and glyburide, you shouldn’t be near a prescription pad.
Michael Ochieng
December 23, 2025 AT 00:49From India, I’ve seen how generic drugs save lives here. But I also saw a technician in a small clinic give a patient the wrong version of metformin because the pill looked different. We need global standards. Not 120 in Texas, 180 in California. That’s absurd. We’re all saving lives the same way.
Erika Putri Aldana
December 23, 2025 AT 18:02Why do we even care? Big Pharma just wants us to memorize stuff so they can keep selling the same pills under new names. It’s all a scam. I’ve seen techs get fired for mixing up drugs… but the companies? They just hire another one. The system is rigged.
Sandy Crux
December 25, 2025 AT 02:25One must question the very epistemological foundations of this 'Top 200' list-how arbitrary, how culturally biased, how insufficiently nuanced. To reduce pharmaceutical knowledge to a checklist is to misunderstand the ontological complexity of pharmacotherapy. One cannot 'learn' a drug. One must *sit with it*.
Hannah Taylor
December 25, 2025 AT 17:31u/PharmTech2020? That’s not a real person. That’s a bot made by PTCB to scare new techs. I’ve been in this job 10 years and never had an error. They just want you to buy their $50 course. The VA doesn’t even require all that. It’s all a money grab.
Jason Silva
December 27, 2025 AT 06:50Bro. I used to suck at this. Then I started using Epocrates every morning while brushing my teeth. Now I know every pill in the drawer. 🤘 Also, if you’re still using flashcards, you’re doing it wrong. AI tools are the future. Walmart’s system cut errors by 22%. That’s not luck. That’s science.
mukesh matav
December 27, 2025 AT 10:44My uncle was a pharmacy tech in Mumbai. He never saw brand names. Just generics. He learned by asking the pharmacist, not memorizing. Maybe we don’t need all this testing. Maybe we need more mentorship.
Peggy Adams
December 28, 2025 AT 11:51they say 7000 deaths a year from med errors but i bet half of those are from doctors writing bad scripts. why is it always the techs getting blamed? i saw a doc write 'morphine' and mean 'morphine sulfate' and the tech gave it anyway. who's the real problem here?
Theo Newbold
December 28, 2025 AT 22:40Let’s be honest: this whole competency push is just corporate liability theater. The real issue? Understaffed pharmacies. Overworked techs. No time to double-check. They want you to memorize 200 drugs so they don’t have to hire more people. It’s not about safety. It’s about profit.