When you’re struggling with depression or anxiety, the idea of taking a medication like an SSRI can feel overwhelming. You’ve probably heard people say they ‘fixed’ their mood, or worse, that they ‘numbed’ their emotions. The truth is more complicated-and more human. SSRIs don’t magically turn you into someone else. They help your brain rewire itself, slowly, over weeks. And while they work for millions, they’re not without real, sometimes tough, side effects.
What SSRIs Actually Do in Your Brain
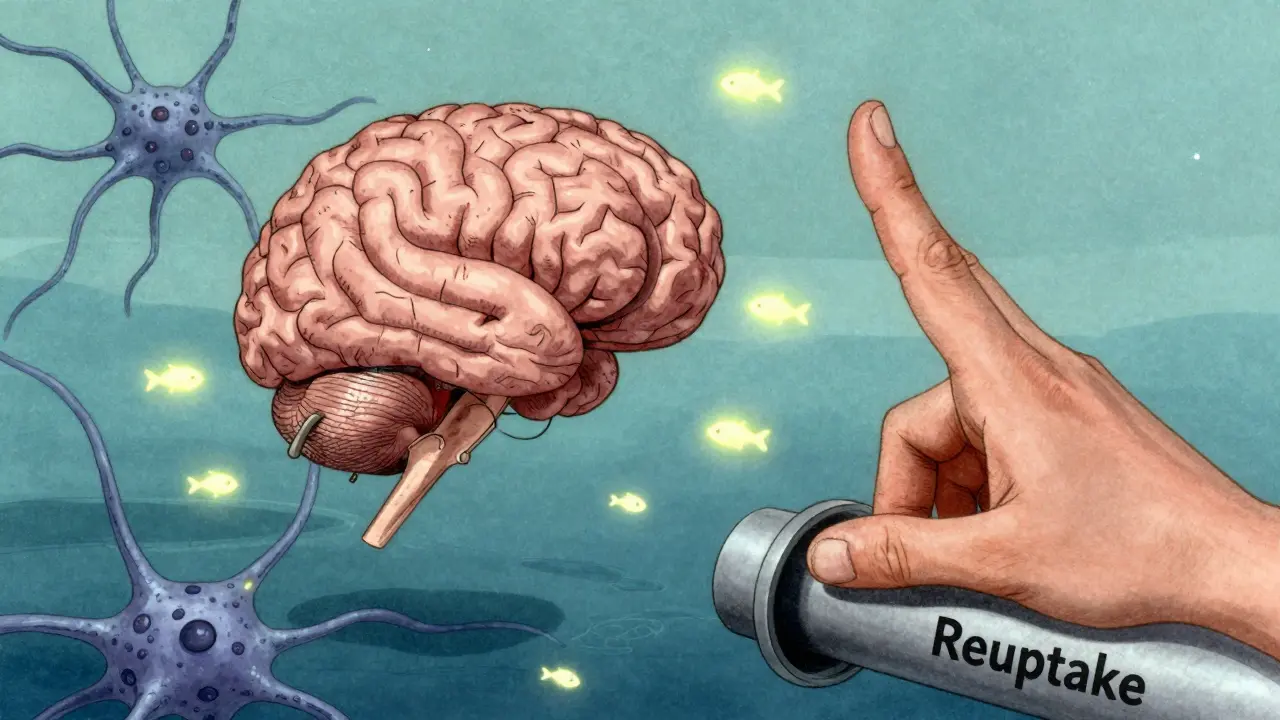
SSRIs stand for selective serotonin reuptake inhibitors. That’s a mouthful, but here’s what it means in plain terms: your brain uses serotonin to send signals between nerve cells that affect mood, sleep, and anxiety. After serotonin does its job, it’s usually sucked back up into the sending cell-like a recycling system. SSRIs block that recycling. That means more serotonin stays floating in the space between nerve cells, giving your brain more of it to work with.
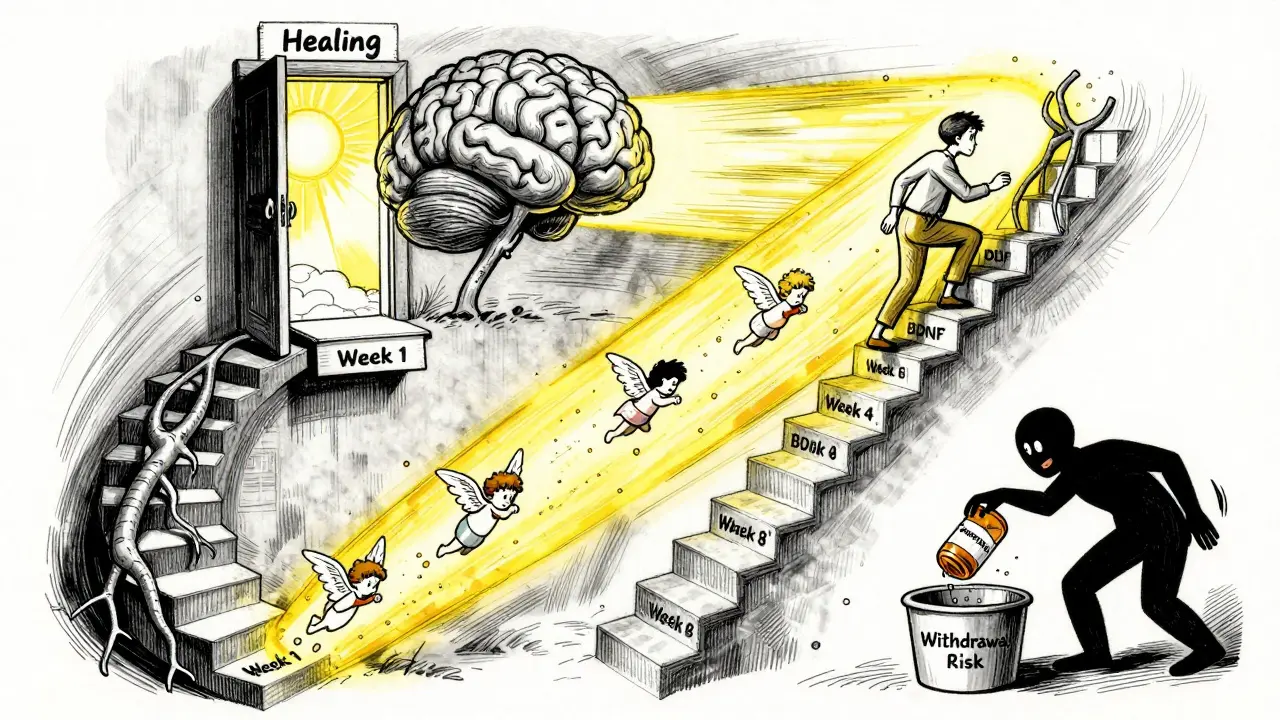
This isn’t like flipping a switch. You don’t feel better right away. In fact, within an hour of taking your first pill, serotonin levels rise-but you won’t notice a thing. Why? Because your brain needs time to adapt. The real change happens over 4 to 6 weeks. During that time, your brain’s serotonin receptors start to adjust. One key mechanism is the desensitization of 5HT1A autoreceptors in the raphe nuclei. Think of these as brakes on serotonin production. When they quiet down after a few weeks, your brain starts firing serotonin more freely, and that’s when mood improvement begins.
It’s not just about serotonin levels. Studies show SSRIs also boost brain-derived neurotrophic factor, or BDNF-a protein that helps brain cells grow and connect. After 8 weeks of treatment, responders show a 25-30% increase in BDNF. This suggests SSRIs don’t just correct a chemical imbalance-they help your brain heal itself.
The Six Main SSRIs You’ll Encounter
There are six SSRIs approved in the U.S. Each has slight differences in how long they last in your body and how they’re processed. Here’s what you’re likely to be prescribed:
- Fluoxetine (Prozac): Longest half-life-up to 16 days for its active metabolite. This means if you miss a dose, you’re less likely to feel withdrawal. Often used for depression, OCD, and bulimia.
- Sertraline (Zoloft): Most commonly prescribed. Good balance of effectiveness and tolerability. Often first choice for depression and anxiety.
- Escitalopram (Lexapro): The active form of citalopram. Often better tolerated, with fewer side effects. High user satisfaction ratings.
- Citalopram (Celexa): Similar to escitalopram but slightly more likely to cause heart rhythm changes at high doses.
- Paroxetine (Paxil): Shortest half-life-21 hours. This makes it more likely to cause withdrawal symptoms if you stop suddenly. Also has the strongest link to weight gain and sexual side effects.
- Fluvoxamine (Luvox): Less commonly used in the U.S., but popular in Europe for OCD and anxiety. Also has some anti-inflammatory effects.
Doctors usually start with sertraline or escitalopram because they’re effective and have fewer side effects. But your body reacts differently than someone else’s. That’s why finding the right one can take trial and error.
Side Effects: What Most People Experience
Side effects are common-especially in the first 2 to 4 weeks. About 74% of people report them, according to user surveys. But many fade over time.
- Upset stomach: Nausea, diarrhea, or constipation. Usually improves within a couple of weeks. Taking the pill with food helps.
- Insomnia or drowsiness: Some SSRIs energize you (like fluoxetine), others make you tired (like paroxetine). Timing your dose can help-morning for energizing ones, night for sedating ones.
- Sexual side effects: This is the most persistent issue. Up to 58% of users report reduced libido, trouble getting aroused, or delayed orgasm. It’s not just ‘in your head.’ It’s a real chemical effect. Some people switch medications or add low-dose bupropion to counteract this.
- Emotional blunting: Some people say they feel ‘flat’-less joy, less sadness. It’s not depression, but a dulling of emotional range. This affects about 42% of long-term users. It’s not always discussed, but it’s real.
- Weight changes: Paroxetine is most linked to weight gain. Others, like fluoxetine, may cause slight weight loss early on. Long-term, most people stabilize.
It’s important to know: side effects don’t mean the drug isn’t working. They often mean your body is adjusting. If they’re unbearable, talk to your doctor. Don’t quit cold turkey.

Discontinuation Syndrome: The Hidden Risk
Stopping an SSRI suddenly can cause what’s called discontinuation syndrome. It’s not addiction. It’s your nervous system reacting to the sudden drop in serotonin.
Symptoms include:
- Dizziness or vertigo
- Electric shock sensations in the head (sometimes called ‘brain zaps’)
- Flu-like symptoms
- Increased anxiety or irritability
- Sleep disturbances
These are worst with short-acting SSRIs like paroxetine and sertraline. Fluoxetine, because it lingers in your system, rarely causes this. The key is tapering. Never stop on your own. A slow reduction over 4-8 weeks, under medical supervision, prevents most of these symptoms.
Who Shouldn’t Take SSRIs?
SSRIs are safe for most people-but not everyone.
- People under 25: The FDA requires a black box warning because SSRIs slightly increase suicidal thoughts in teens and young adults during the first month. This doesn’t mean they cause suicide-it means close monitoring is needed.
- Those on MAOIs: Combining SSRIs with MAOIs (like phenelzine) can cause serotonin syndrome-a rare but dangerous buildup of serotonin that can be fatal.
- People with certain heart conditions: Citalopram and escitalopram can affect heart rhythm at high doses. A baseline ECG may be needed.
- Those with bipolar disorder: SSRIs can trigger mania if not paired with a mood stabilizer.
Also, if you’re pregnant or breastfeeding, talk to your doctor. Some SSRIs cross the placenta, but untreated depression also carries risks. The decision is personal and should be made with your care team.
How Effective Are They Really?
Let’s be honest: SSRIs aren’t magic. The STAR*D trial, the largest depression study ever done, found only about 30% of people went into full remission after the first SSRI. That means two out of three people need to try something else-either a different SSRI, a different class of antidepressant, therapy, or a combination.
But here’s what’s important: SSRIs are the most tolerated class of antidepressants. Compared to older drugs like tricyclics, they’re far safer in overdose and cause fewer dry mouth, dizziness, or heart problems. They’re also the most studied. For moderate to severe depression, they’re more effective than placebo. For mild depression, therapy alone might be just as good.
And for anxiety disorders-panic disorder, social anxiety, OCD-SSRIs are often the gold standard. They work better than most other medications for these conditions.
The Big Debate: Is the Serotonin Theory Wrong?
You’ve probably heard the claim: ‘Depression isn’t caused by low serotonin.’ And you’re right to question it. The idea that depression = low serotonin has been oversimplified for decades.
Research shows only 25-30% of people with depression actually have measurable serotonin deficiencies. So why do SSRIs work for so many?
The answer might be in the brain’s response, not the starting point. Dr. Helen Mayberg’s brain imaging studies show that SSRIs normalize activity in the subcallosal cingulate cortex-a region linked to emotional regulation. Even if serotonin isn’t the root cause, SSRIs help the brain reorganize how it handles stress and emotion.
Think of it like a broken door hinge. You don’t fix the hinge by adding more oil-you fix it by adjusting the alignment. SSRIs might not fix the cause of depression, but they help the brain function better again.
What Comes Next?
Science is moving fast. New research is identifying genetic markers in the SLC6A4 gene that predict who will respond to SSRIs-with 78% accuracy. In the next 5 years, we may see blood tests or genetic screens guide which SSRI you get.
Also, new drugs like vilazodone (Viibryd) combine serotonin reuptake inhibition with partial receptor activation. Early results show 15% fewer sexual side effects.
And for those who don’t respond? Combination therapy-SSRIs plus talk therapy-is the most proven path forward. CBT, in particular, helps rewire thought patterns that SSRIs alone can’t touch.
SSRIs aren’t perfect. But they’ve helped millions get back to living. If you’re considering them, give them time. Track your symptoms. Talk to your doctor about side effects. And remember: you’re not broken. You’re healing.
kenneth pillet
January 19, 2026 AT 07:53Been on sertraline for 3 years. Nausea faded after 2 weeks. Sex drive took 6 months to come back. Worth it.
Jodi Harding
January 19, 2026 AT 19:29They don’t fix depression. They just make you too tired to care about being depressed. That’s not healing. That’s surrender.
Wendy Claughton
January 20, 2026 AT 20:08I love how this post doesn’t sugarcoat it. 🌱 I was terrified to start SSRIs, but after 10 weeks, I cried for the first time in years-not from sadness, but because I could feel again. Not numb. Just… human.
Stacey Marsengill
January 21, 2026 AT 21:40Of course it’s ‘chemical imbalance’ nonsense. Big Pharma paid your doctor to push this. You’re being manipulated. Stop taking poison.
Praseetha Pn
January 22, 2026 AT 22:42SSRIs are a CIA mind control program disguised as medicine. Look up the MKUltra files. They’ve been testing this on civilians since the 50s. Your brain isn’t broken-it’s being hacked.
Chuck Dickson
January 23, 2026 AT 15:05Hey-first time on escitalopram? Give it 6 weeks. Don’t quit at week 2. I was ready to throw in the towel… then one morning, I actually wanted coffee. No joke. That’s the moment. You’ll know it.
Kristin Dailey
January 24, 2026 AT 12:17Why are we even letting people take these? America’s gone soft. Just get outside. Lift weights. Stop looking for a pill to fix your life.
rachel bellet
January 24, 2026 AT 12:53The BDNF upregulation data is statistically significant but clinically marginal. The effect size (Cohen’s d = 0.32) doesn’t justify first-line monotherapy for mild-to-moderate MDD. You’re conflating neuroplasticity with therapeutic efficacy.
Pat Dean
January 26, 2026 AT 00:38I tried fluoxetine. Felt like a zombie. My husband said I stopped laughing. Then I quit cold turkey. Brain zaps for two weeks. Worth it? No. Never again.
Jay Clarke
January 26, 2026 AT 17:09They say SSRIs help you ‘rewire’ your brain… but what if your brain’s just trying to tell you your life sucks? Maybe you don’t need a chemical fix-you need to leave your job, end the toxic relationship, stop pretending you’re okay.
Selina Warren
January 28, 2026 AT 00:44My therapist said SSRIs are like training wheels. They don’t fix the bike-but they let you ride until you learn to balance. I’m off now. 18 months. Still feel like me. Not a robot. Not numb. Just… free.
Naomi Keyes
January 29, 2026 AT 09:31While the pharmacokinetic profiles of SSRIs are well-documented, it is critically important to note that the 5HT1A autoreceptor desensitization hypothesis remains a theoretical construct, not a proven mechanism. Moreover, the STAR*D trial’s remission rates are misleadingly reported-only 27.5% achieved remission after the first treatment step, and attrition exceeded 50% by step three. The placebo response rate in antidepressant trials is consistently 35-40%, rendering the clinical significance of SSRIs highly questionable. Additionally, the promotion of BDNF as a biomarker is speculative; no longitudinal studies have validated its predictive value for treatment response. One must also consider the ethical implications of prescribing long-term psychopharmacology to populations with limited access to psychotherapy-this is not medicine, it is triage.
Chuck Dickson
January 31, 2026 AT 08:43Bro, I read your comment and I’m not mad. I get it-you’re smart. But I met a girl at the grocery store last week who told me she cried for the first time in 4 years after 6 weeks on sertraline. She didn’t know what BDNF was. She just knew she wanted to hug her kid again. Sometimes the science doesn’t need to be perfect to be real.