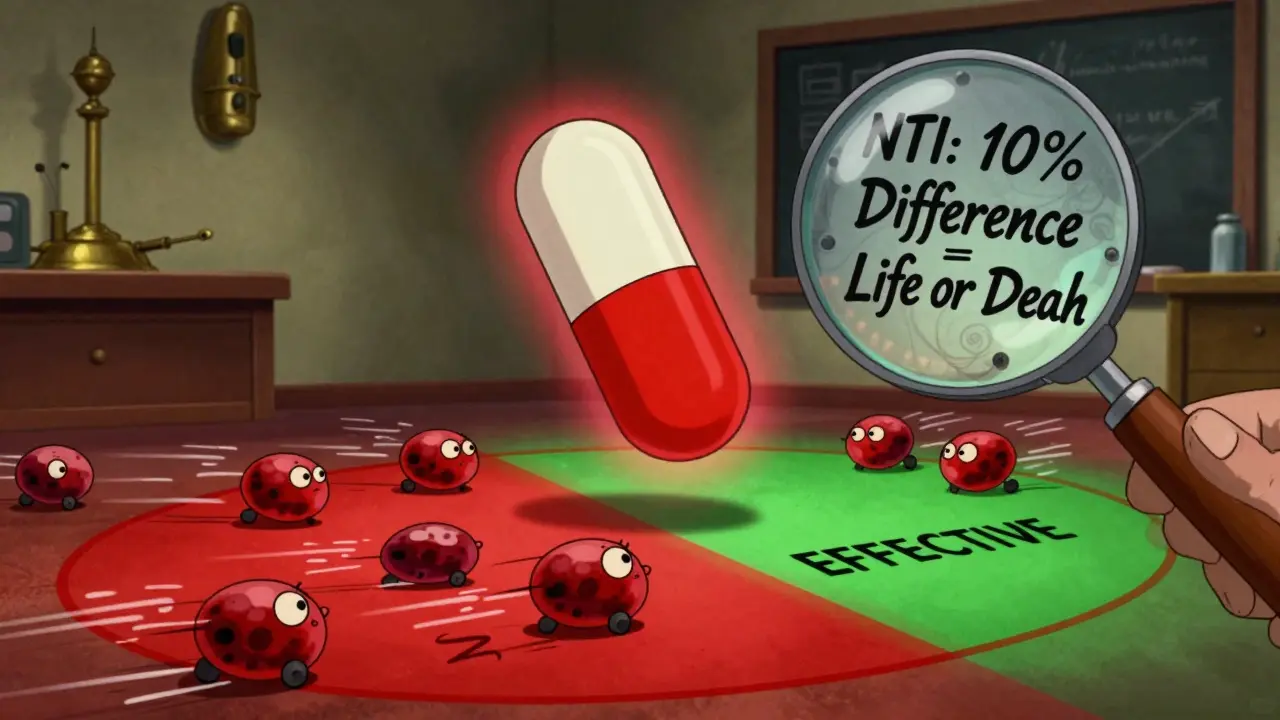
When you take a pill for a serious condition-like warfarin to prevent blood clots, levothyroxine for thyroid function, or digoxin for heart rhythm-even a tiny change in how much drug enters your bloodstream can be dangerous. That’s why narrow therapeutic index drugs have special rules. These aren’t your average generics. They’re high-stakes medications where even a 10% difference in absorption could mean the difference between effective treatment and life-threatening side effects.
What Makes a Drug Have a Narrow Therapeutic Index?
A narrow therapeutic index (NTI) means the gap between a drug’s effective dose and its toxic dose is very small. The FDA uses a cutoff of a therapeutic index ≤ 3 to define these drugs. That means if the dose that works is 10 mg, the dose that starts causing harm might be just 30 mg or less. There’s almost no room for error.
These drugs aren’t rare. About 35 medications fall into this category in the U.S., and they account for $45 billion in annual sales. Common examples include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Digoxin (heart medication)
- Phenytoin (anti-seizure)
- Tacrolimus (organ transplant rejection blocker)
- Lithium carbonate (mood stabilizer)
For decades, doctors monitored blood levels of these drugs manually. Patients on warfarin got frequent INR tests. Those on phenytoin had blood draws every few weeks. That was the safety net. But when generic versions started appearing, regulators had to ask: Can we trust a pill made by a different company to behave exactly the same?
Standard Bioequivalence Rules Don’t Cut It
For most generic drugs, regulators accept a 25% range: if the generic delivers 80% to 125% of the brand-name drug’s exposure in the blood, it’s considered equivalent. That’s called the 80.00-125.00% bioequivalence window. It works fine for antibiotics, painkillers, or blood pressure meds where small differences don’t matter much.
But for NTI drugs? That range is too wide. A 125% exposure might push a patient into toxicity. An 80% exposure might let a clot form. So regulators had to tighten the rules.
The FDA, EMA, and Health Canada all responded-but differently.
How Different Regulators Handle NTI Drugs
The FDA’s approach is the most complex-and the most scientifically detailed. Since 2021, they require generic NTI drugs to pass three tests:
- Reference-Scaled Average Bioequivalence (RSABE): The acceptable range isn’t fixed. It expands or contracts based on how much the original drug varies from person to person. If the brand-name drug has high variability (say, 15%), the generic can vary a bit more too. But if the brand is super consistent (say, 5%), the generic must match it almost perfectly.
- Variability Comparison: The generic can’t be more variable than the brand. If the brand’s blood levels fluctuate a little between doses, the generic must stay within that same range. This stops companies from making a drug that’s average but unpredictable.
- Unscaled Average Bioequivalence: Even with the scaled approach, the generic must still fall within the traditional 80-125% range. It’s a backup safety net.
This approach requires bigger studies-usually 36 to 54 volunteers instead of 24. It also costs more: $500,000 to $1 million per drug, compared to $300,000-$700,000 for regular generics.
Meanwhile, the European Medicines Agency (EMA) uses a simpler method: a fixed 90-111% window for both AUC and Cmax. Health Canada uses 90.0-112.0% for AUC. These are stricter than the standard 80-125%, but they don’t adjust for variability. That means even a low-variability drug like levothyroxine gets the same tight limits as a high-variability one like phenytoin.
Why the difference? The FDA’s method is more flexible and scientifically precise. But it’s harder to run. The EMA and Health Canada went for simplicity and consistency. Each system has trade-offs.
Why This Matters for Patients
Patients don’t always know they’re taking an NTI drug. But they feel the consequences if something goes wrong.
In 2017, a study in the American Journal of Transplantation followed hundreds of kidney transplant patients switched from brand-name tacrolimus to a generic version. Using the FDA’s stricter bioequivalence criteria, researchers found no increase in rejection rates or toxicity. That’s a big deal-transplant patients can’t afford even a small dip in drug levels.
Another study in Circulation: Cardiovascular Quality and Outcomes in 2019 looked at warfarin users. They compared brand and generic versions and found no difference in stroke, bleeding, or hospitalization rates. That’s reassuring. But those results only came because the generics passed the tighter tests.
Without those rules, patients could be at risk. One 2021 study in JAMA Internal Medicine found that only 68% of NTI drugs in the U.S. market were generic-compared to 90% for other drugs. Why? Because manufacturers were scared off by the cost and complexity of proving equivalence. Some doctors still prescribe brand names out of caution, even when generics are approved.
Industry Pushback and the Cost of Safety
Not everyone agrees the FDA’s rules are perfect. Some experts, like Dr. Lawrence Lesko, worry the high costs and complex testing could block good generics from reaching the market. If only one company can afford to run a $1 million study, you get less competition-and higher prices.
But others, like Dr. Leslie Benet from UCSF, argue that the FDA’s approach is the gold standard. It doesn’t just assume equivalence-it proves it using real pharmacokinetic data. The variability test, in particular, catches generics that might look fine on average but behave unpredictably in real patients.
The FDA acknowledges the tension. They’re working on a new system to classify NTI drugs more objectively. Right now, they decide case by case, based on clinical experience. But starting in 2024, they plan to use quantitative thresholds-like the therapeutic index ≤ 3 rule-to make classifications more consistent.
What’s Next for NTI Drugs?
By 2026, we might see more alignment between the FDA, EMA, and Health Canada. If regulators agree on a common framework, generic manufacturers won’t have to run three different studies for the same drug. That could cut costs by 15-20%, according to McKinsey & Company’s 2023 analysis.
There’s also a push to create a public, official list of NTI drugs. Right now, the FDA doesn’t publish one. Instead, they issue guidance for specific drugs as they come up. That creates confusion. A manufacturer might spend millions developing a generic for a drug they think is NTI-only to find out the FDA hasn’t classified it that way yet.
Meanwhile, patients and prescribers are slowly gaining confidence. Real-world data keeps proving that approved generic NTI drugs are safe. The key word is approved. Not all generics are equal. Only those that passed the strict bioequivalence tests should be trusted.
What Should You Do as a Patient?
If you’re on an NTI drug:
- Know your medication. Ask your pharmacist or doctor if it’s a narrow therapeutic index drug.
- Don’t switch brands or generics without talking to your provider. Even if two generics are both approved, switching between them can cause small fluctuations.
- Stick to one pharmacy. Different pharmacies might stock different generics. Consistency matters.
- Keep up with blood tests. For warfarin, lithium, or phenytoin, regular monitoring is still essential-even with approved generics.
There’s no need to fear generics. But you do need to be informed. The stricter rules exist because the stakes are high. And when your life depends on a pill working just right, you want the best possible guarantee.
What does 'narrow therapeutic index' mean?
A narrow therapeutic index means the difference between a drug’s effective dose and its toxic dose is very small. Even small changes in how much of the drug enters your bloodstream can lead to treatment failure or serious side effects. Drugs like warfarin, levothyroxine, and digoxin are classic examples.
Why are bioequivalence requirements stricter for NTI drugs?
Standard bioequivalence limits (80-125%) are too wide for NTI drugs. A 25% variation could push a patient into toxicity or cause the drug to stop working. Stricter limits-like 90-111% or the FDA’s reference-scaled approach-ensure that generic versions behave nearly identically to the brand-name drug, reducing the risk of harm.
How does the FDA’s approach differ from the EMA’s?
The FDA uses a three-part test: reference-scaled bioequivalence (which adjusts limits based on variability), a comparison of variability between brand and generic, and a fallback to the standard 80-125% range. The EMA uses a fixed 90-111% window for all NTI drugs, regardless of how variable the original drug is. The FDA’s method is more precise but more complex and expensive to implement.
Are generic NTI drugs safe?
Yes, if they’ve passed the stricter bioequivalence requirements. Real-world studies on generic tacrolimus, warfarin, and phenytoin show no increase in adverse events or treatment failures compared to brand-name versions. The key is that these generics had to meet tighter standards before approval.
Why aren’t more NTI drugs available as generics?
Because the studies to prove bioequivalence are expensive ($500K-$1M) and complex. Many manufacturers avoid NTI drugs because the return on investment is uncertain. This has kept generic market share for NTI drugs around 68%, compared to 90% for other drugs.
Should I avoid switching from brand to generic for NTI drugs?
Not necessarily. If your generic was approved under the FDA’s or EMA’s stricter rules, it’s safe. But avoid switching between different generic brands unless your doctor approves it. Even approved generics can have minor differences in how they’re absorbed. Consistency matters most with NTI drugs.
jefferson fernandes
January 13, 2026 AT 04:19Let me be clear: this isn't just about pills-it's about trust. When your life depends on a drug working exactly right, you don't want some factory in India or China cutting corners because they think 'close enough' is good enough. The FDA's three-part test? That's not bureaucracy-that's basic human decency.
Acacia Hendrix
January 13, 2026 AT 23:44It's fascinating how the pharmacokinetic variance in NTI drugs necessitates a reference-scaled bioequivalence paradigm, particularly when the intra-subject coefficient of variation exceeds 30%. The EMA's fixed interval approach is statistically naive-it fails to account for the nonlinear absorption dynamics inherent in drugs like tacrolimus. We're not talking about ibuprofen here.
lucy cooke
January 14, 2026 AT 16:13People don't realize how much power Big Pharma holds over who lives and who dies. They let generics in only when it's profitable-otherwise, they keep you hooked on brand-name drugs that cost $500 a month. This isn't science-it's capitalism with a stethoscope.
James Castner
January 15, 2026 AT 11:05Consider this: we regulate the purity of our water, the safety of our bridges, the accuracy of our scales-yet for decades, we allowed life-saving medications to be substituted with products that could vary by 25% in absorption. That’s not innovation. That’s negligence. The FDA’s updated framework doesn’t just protect patients-it restores dignity to the science of medicine. This is what rigorous, patient-centered regulation looks like.
mike swinchoski
January 15, 2026 AT 17:29Why do we even bother with generics? Just give me the brand name. I don't care how much it costs. I've seen people die because some cheap pill didn't work right. End of story.
Adam Rivera
January 16, 2026 AT 04:15As someone who's been on levothyroxine for 12 years, I switched to a generic last year after my insurance forced it. No issues. No weird symptoms. My TSH stayed perfect. The system works-if you pick one that's actually been tested right. Don't panic, just ask your pharmacist which one it is.
Rosalee Vanness
January 16, 2026 AT 07:50I used to be terrified of switching generics-until I started reading the studies. Real data, not fear-mongering. The 2019 Circulation paper? That’s the quiet hero of this whole story. It didn’t make headlines, but it saved lives. And now, more people are starting to trust the science instead of the scary stories. That’s progress.
Trevor Davis
January 16, 2026 AT 18:33Y’all are overthinking this. I'm a nurse. I've seen patients crash because they got switched to a generic that didn't sit right. One guy went into atrial fibrillation after switching from brand to generic digoxin. His wife cried in my office. The FDA’s rules? Good. But they’re not enough. We need a national registry. Track every switch. Every blood level. Every outcome. Or people are gonna keep dying.
John Tran
January 17, 2026 AT 20:45So like… if the brand name drug has a lot of variation between people, then the generic can have more variation too? That sounds like saying ‘if the original is messy, the copy can be messy too’… which is weird. Like, shouldn’t we want the copy to be *better*? Also, I think I spelled ‘bioequivalence’ wrong. But you get my point.
Jesse Ibarra
January 19, 2026 AT 16:53Let’s be honest: the FDA’s rules are a joke. $1 million per drug? That’s a tax on competition. It’s not about safety-it’s about protecting the brand-name monopolies. If you can’t afford to play, you don’t get to play. That’s not science. That’s corporate fascism.
laura Drever
January 21, 2026 AT 05:0268% generic penetration? Pathetic. And you wonder why US drug prices are insane. This whole system is rigged. No one cares about patients. Only profits. And the ‘strict rules’? Just a cover. Same old game.
Randall Little
January 22, 2026 AT 04:29So the FDA’s approach is more precise but more expensive… and the EMA’s is simpler but less nuanced. Interesting. So what happens when a generic passes the EMA’s 90-111% test but fails the FDA’s? Does it get sold in the US? Or is it banned? Because that’s the real question nobody’s asking.
Pankaj Singh
January 23, 2026 AT 15:53You Americans think you invented medicine. We’ve been using generics for decades in India without a single death. Your rules are overkill. Your drugs are overpriced. Your system is broken. Fix it before you lecture the world.
Robin Williams
January 25, 2026 AT 00:12So… if your pill is supposed to be a magic bullet but the generic version is like… a magic buckshot? That’s wild. I get why they’re scared. But also-why not just make the brand cheaper? Why punish the people who need it most? Just saying.