What Is Medication-Induced Delirium?
Medication-induced delirium is a sudden, fluctuating state of confusion that happens when certain drugs disrupt brain function in older adults. It’s not dementia. It’s not just being tired. It’s a medical emergency that can develop in just hours after starting or changing a medication. Older adults are especially vulnerable because their brains are more sensitive to drug effects. Their bodies also process medicines slower, so even normal doses can build up and cause trouble.
Think of it like this: your brain runs on chemicals. One of the most important is acetylcholine-it helps with memory, attention, and staying alert. Many common medications block this chemical. When that happens, the brain stumbles. People suddenly forget where they are, mix up day and night, or become agitated for no reason. Sometimes they just sit there, quiet and withdrawn, staring blankly. That’s not normal aging. That’s delirium.
The Most Dangerous Medications
Not all drugs cause this. But some are far more likely to trigger it. The biggest culprits fall into three groups: anticholinergics, benzodiazepines, and certain opioids.
Anticholinergic drugs are the number one cause. These include common over-the-counter sleep aids like diphenhydramine (Benadryl), bladder control pills like oxybutynin, and even some antidepressants like amitriptyline. The American Geriatrics Society’s Beers Criteria® lists 56 of these as high-risk for seniors. Every extra anticholinergic drug you take? It adds up. Three or more? That’s a 4.7 times higher chance of delirium.
Benzodiazepines like lorazepam (Ativan) and diazepam (Valium) are next. They’re often given for anxiety or sleep, but they slow down the brain too much. Studies show they triple the risk of delirium in hospitals. Even short-term use can trigger it. And if someone stops them suddenly? That can cause withdrawal delirium-just as dangerous.
Opioids like morphine and meperidine are tricky. Pain relief is essential, but some opioids are worse than others. Meperidine is especially risky because its breakdown product messes with brain signals. Hydromorphone is a safer choice-it causes 27% less delirium at the same pain-killing dose.
How It Shows Up: The Hidden Signs
Most people think delirium means shouting, flailing, or hallucinating. That’s only one type: hyperactive delirium. But in older adults, it’s usually the opposite.
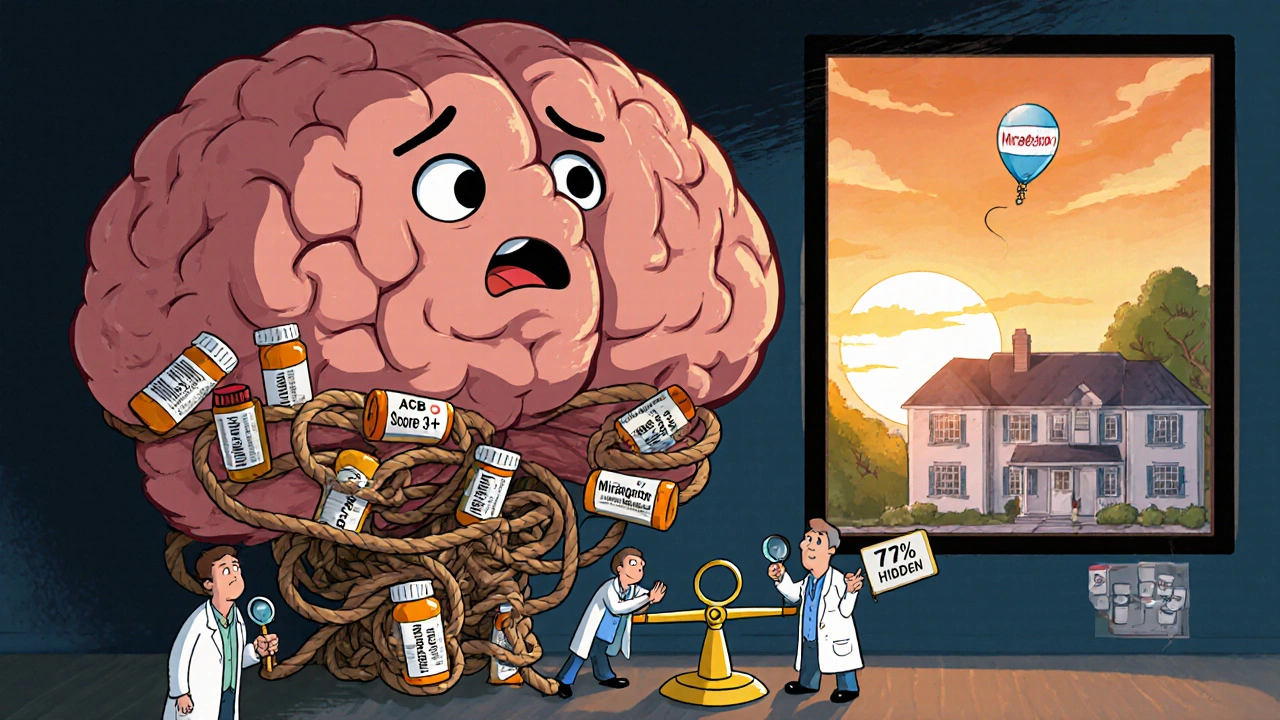
Hypoactive delirium-the quiet kind-is the most common. It affects 72% of cases. The person seems calm, maybe even sleepy. They don’t respond when spoken to. They skip meals. They don’t recognize family. They might sit for hours without moving. Families often mistake this for depression, dementia, or just getting older. That’s why it’s missed 70% of the time.
Here’s what to watch for:
- Sudden change in personality-someone who was alert and chatty becomes withdrawn
- Confusion that comes and goes-better in the morning, worse at night
- Difficulty focusing-can’t follow a simple conversation
- Forgetfulness beyond normal aging-doesn’t remember what they ate for breakfast
- Strange behavior-picking at blankets, talking to imaginary people, or staring into space
Family members often say, “It happened overnight.” And it did. A new painkiller. A new sleep aid. A dose change. Within 24 to 72 hours, things go sideways.
Why This Happens So Often
It’s not just bad prescribing. It’s systemic. Older adults often take five, six, even ten medications. Each one adds risk. Doctors may not know about the anticholinergic burden. Pharmacists don’t always flag it. Hospitals don’t screen for it.
And then there’s the myth: “It’s just dementia getting worse.” But delirium is different. Dementia is slow. Delirium is sudden. If someone with dementia suddenly becomes more confused, it’s likely not their disease progressing-it’s a drug.
People over 85 are 2.3 times more likely to get it than those in their 60s. Those with existing dementia? Their delirium lasts nearly twice as long-8.2 days on average. And once it happens, their recovery slows. They’re more likely to end up in a nursing home. Their risk of dying within a year doubles.
How to Prevent It
The good news? Medication-induced delirium is one of the most preventable hospital-acquired conditions. You don’t need fancy tech. You just need awareness and action.
1. Review every medication. Ask: Is this still needed? Could it be replaced? Use the Anticholinergic Cognitive Burden Scale (ACB). A score of 3 or higher means high risk. Many common meds-like diphenhydramine, oxybutynin, and trazodone-score high. Swap them out. Use loratadine instead of Benadryl. Use mirabegron instead of oxybutynin for bladder control.
2. Avoid benzodiazepines unless absolutely necessary. For anxiety or sleep? Try non-drug options first: light exposure, routine, calming music. If meds are needed, use the shortest-acting option (lorazepam) for the shortest time possible. Never use them for routine sedation.
3. Manage pain smarter. Don’t jump straight to opioids. Use acetaminophen first. Add physical therapy, heat packs, or massage. Studies show this cuts opioid use by 37%-and that cuts delirium risk.
4. Use screening tools. Hospitals that use the Confusion Assessment Method (CAM) see 32% fewer cases. Ask: Is the person alert? Can they focus? Are they thinking clearly? If not, suspect delirium.
5. Educate caregivers and staff. Only 35% of hospital staff correctly spot hypoactive delirium. That’s unacceptable. Training saves lives.
What to Do If You Suspect It
If you notice sudden confusion in an older adult, don’t wait. Don’t assume it’s just aging. Act.
- Stop all non-essential medications immediately-especially anticholinergics and benzodiazepines
- Call the doctor. Say: “I think this might be medication-induced delirium.”
- Bring a full list of all meds, including supplements and OTC drugs
- Check for other triggers: infection, dehydration, low sodium
Don’t be afraid to push. Many doctors dismiss it as “just confusion.” But if it’s drug-related, stopping the medicine often reverses it in days.
Real Change Is Happening
There’s progress. The FDA now requires stronger warnings on anticholinergic labels. The National Institute on Aging is funding real-time drug risk alerts in electronic health records. Some hospitals use AI tools that scan medication lists and flag high-risk combos with 84% accuracy.
But change is slow. In 2023, 43% of hospitals still routinely prescribe high-risk drugs to seniors. Only 18% check anticholinergic burden systematically.
This isn’t just about one person. It’s about millions. In the U.S., over 2.6 million older adults get medication-induced delirium each year. It adds $164 billion to healthcare costs. And the number will rise as the population ages.
Final Thought: Your Voice Matters
You don’t need to be a doctor to prevent this. You just need to ask questions. If your parent or grandparent is in the hospital or starting a new pill, ask: “Could this cause confusion?” “Is there a safer alternative?” “Are we sure they still need this?”
Delirium isn’t inevitable. It’s often caused. And if it’s caused by a drug, it can be undone. The sooner you speak up, the faster recovery can begin.

Gayle Jenkins
November 27, 2025 AT 22:34sharicka holloway
November 29, 2025 AT 16:44Kaleigh Scroger
November 29, 2025 AT 19:14Alex Hess
November 30, 2025 AT 11:09Savakrit Singh
December 2, 2025 AT 06:53Emma louise
December 2, 2025 AT 19:29Elizabeth Choi
December 4, 2025 AT 16:12Jebari Lewis
December 5, 2025 AT 01:40laura lauraa
December 5, 2025 AT 22:24Cecily Bogsprocket
December 6, 2025 AT 22:59Asha Jijen
December 7, 2025 AT 04:30Allison Turner
December 7, 2025 AT 13:12steve stofelano, jr.
December 9, 2025 AT 05:28Emma louise
December 9, 2025 AT 05:54Gayle Jenkins
December 10, 2025 AT 19:09