When someone turns 70, their kidneys don’t work the same way they did at 30. That’s not just a normal part of aging-it’s a medical reality that directly affects how medications work in their body. Around 30% of common drugs prescribed to older adults are cleared by the kidneys. If you don’t adjust the dose based on actual kidney function, you risk toxicity, falls, confusion, or even hospitalization. The problem isn’t that doctors don’t care-it’s that most don’t know which test to use, or worse, they rely on what the computer suggests without thinking.
Why Standard Kidney Tests Fail in Seniors
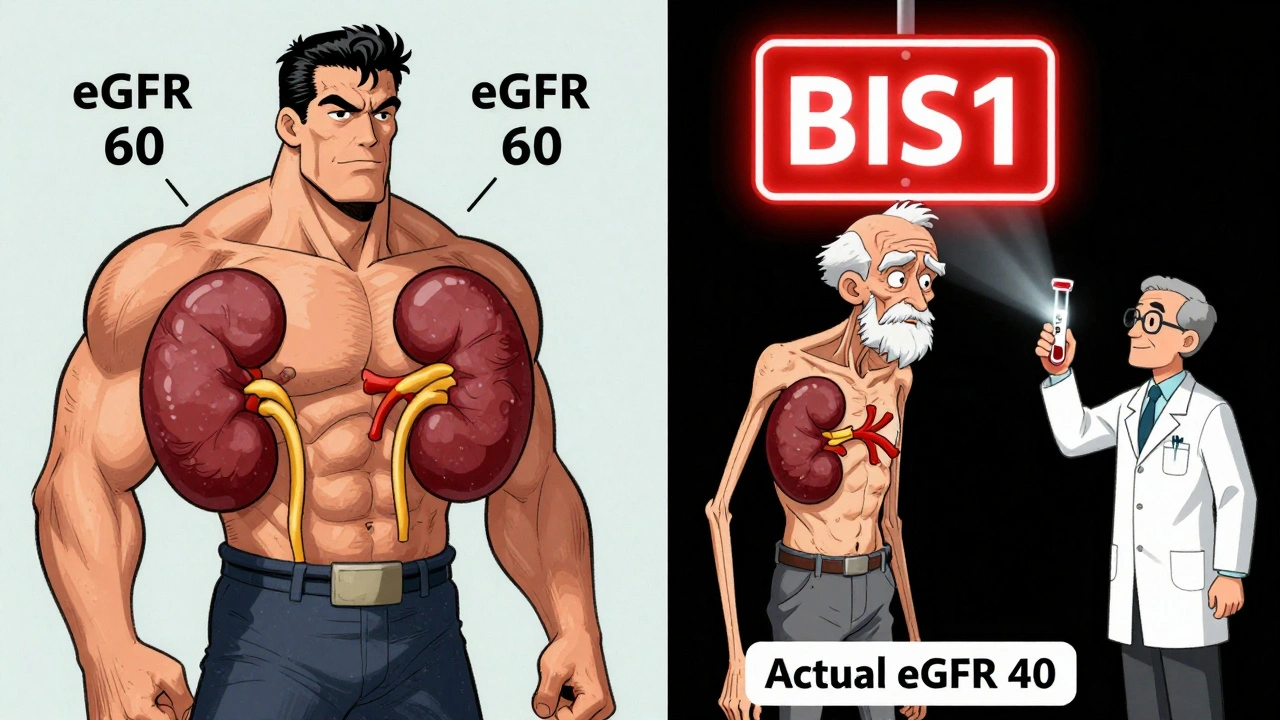
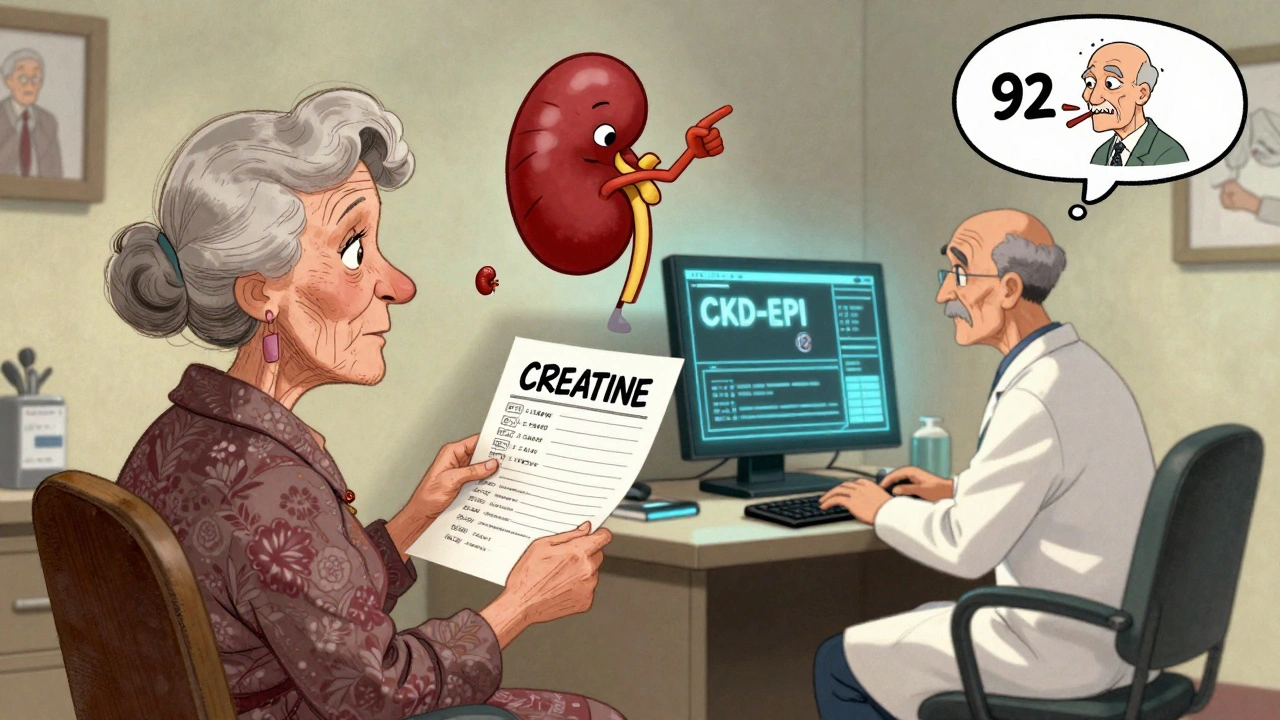
Most clinics still use serum creatinine to estimate kidney function. It’s cheap, fast, and built into every lab order. But here’s the catch: creatinine comes from muscle. As people age, they lose muscle mass-even if they look healthy. A frail 85-year-old woman might have the same creatinine level as a 50-year-old athlete, but her kidneys are far weaker. Using creatinine alone is like judging a car’s fuel efficiency by how much gas is left in the tank, without knowing how big the tank is.The standard equations used to turn creatinine into an estimated GFR (eGFR)-like MDRD and CKD-EPI-were designed for younger, healthier adults. In seniors, they often overestimate kidney function. A 2017 study found that CKD-EPI gave a falsely high reading in 40% of patients over 75 with low muscle mass. That means a doctor might think the kidneys are working at 60 mL/min/1.73m² when they’re actually at 40. If the patient is on a drug like rivaroxaban or digoxin, that 20-point error could be deadly.
Which Equations Actually Work for Older Adults?
Not all equations are created equal. Here’s what the evidence says:- Cockcroft-Gault (CG) with ideal body weight: This is the only formula that includes weight. But using actual body weight in obese or underweight seniors gives wildly wrong results. Studies show switching to ideal body weight reduces dosing errors by 25%. It’s old, but still useful-if done right.
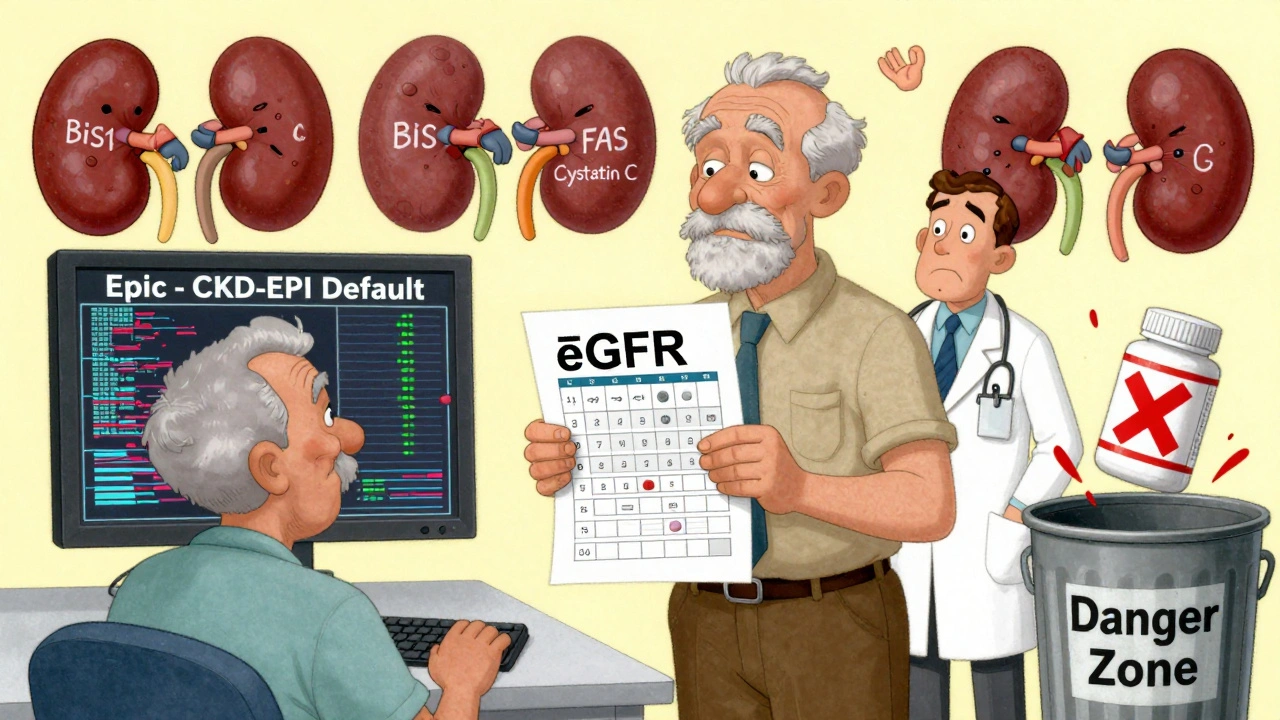
- CKD-EPI: The current standard for most clinics. Works okay for seniors with normal muscle mass, but fails badly in frail, thin, or malnourished patients. It’s fine for general screening, but not for dosing critical drugs.
- BIS1 and FAS: These newer equations were built specifically for older adults. They account for age, sex, and creatinine-but they also factor in how much muscle someone is likely to have. In a 2019 study of 85-year-olds, BIS1 was 95% accurate compared to the gold standard, while CKD-EPI was only 78%. In geriatric clinics, switching from CKD-EPI to BIS1 cut medication errors by 18%.
- Serum cystatin C: This is a protein made by all cells, not just muscle. It’s a better marker for kidney function in seniors with low muscle mass. It costs more-$50-$75 extra-but it’s worth it when the stakes are high. If creatinine says the kidneys are okay, but cystatin C says they’re failing, trust cystatin C.
There’s no single best equation for everyone. The key is matching the tool to the patient. Use BIS1 or FAS for frail, elderly, or underweight seniors. Use CG with ideal body weight for those with obesity or normal muscle mass. Reserve cystatin C for when creatinine looks normal but symptoms suggest kidney trouble.
What to Do When the Numbers Don’t Add Up
Sometimes, the numbers are confusing. A patient has a normal creatinine but is confused, dizzy, or has swelling. That’s a red flag. Don’t ignore it just because the eGFR says “Stage 1” or “Stage 2” kidney disease.Here’s a real-world protocol used in top geriatric clinics:
- Start with BIS1 for anyone over 75, especially if they’re frail, have lost weight, or have multiple chronic conditions.
- If the BIS1 eGFR is between 45-59 mL/min/1.73m² and there’s no protein in the urine, order a serum cystatin C test.
- If cystatin C confirms low kidney function, double-check with a 24-hour urine collection for creatinine clearance-especially before starting drugs like colistin, aminoglycosides, or lithium.
This isn’t routine in most primary care offices. But it’s what happens in places that treat hundreds of elderly patients every year. The difference? They don’t trust the computer. They trust the patient’s body.
How Electronic Health Records Are Making It Worse
Most clinics rely on their EHR system to calculate eGFR automatically. Epic, Cerner, Allscripts-they all use CKD-EPI by default. Even if you’re prescribing a drug that needs precise dosing, the system won’t warn you unless you manually override it.A 2023 survey found that 65% of primary care doctors admit they don’t know which equation their system is using. Forty-two percent just accept the default. That’s dangerous. One pharmacist in a long-term care facility told a Reddit thread: “I override the EHR at least once a week. Last month, it gave a 92-year-old with 35 lbs of muscle the same dose as a 65-year-old weightlifter. She ended up in the ER with kidney failure.”
Some systems are finally changing. Epic now auto-selects BIS1 for patients over 75. But that’s only in big hospitals. Most community clinics still use outdated defaults. If your doctor doesn’t know how to change it, ask. Or better yet, bring your own printout from the National Kidney Foundation’s eGFR calculator-updated November 2023-and ask them to compare it with what the system shows.
Drugs That Need Special Attention
Not all medications are equally risky. Some are fine at any kidney level. Others need strict dosing based on eGFR. Here are the big ones:- Anticoagulants: Dabigatran, rivaroxaban, apixaban-all cleared by kidneys. Overdose = bleeding. Underdose = stroke.
- Diabetes drugs: Metformin is generally safe if eGFR >45, but many doctors stop it too early. New guidelines say you can keep it down to eGFR 30 if the patient is stable.
- Pain meds: Avoid NSAIDs (ibuprofen, naproxen) entirely in seniors with eGFR <60. Use acetaminophen instead.
- Antibiotics: Vancomycin, aminoglycosides, and ciprofloxacin need dose adjustments. Vancomycin toxicity is a leading cause of acute kidney injury in nursing homes.
- Heart meds: Digoxin, amiodarone, and beta-blockers like metoprolol accumulate in kidney failure. Even small changes in eGFR can cause dangerous side effects.
Check your meds. If you’re on more than five, ask your pharmacist: “Which ones depend on my kidneys? What’s my real eGFR?” Most pharmacists in senior care now use BIS1 or CG with ideal body weight. They’re the ones catching the errors before they happen.
What You Can Do Right Now
You don’t need to be a doctor to protect yourself or a loved one. Here’s your action plan:- Ask for your latest serum creatinine and eGFR result. Don’t just accept “normal.” Ask: “Which equation was used?”
- If you’re over 75, frail, or have lost weight, ask: “Should we use BIS1 or cystatin C instead?”
- Review your medication list with your pharmacist. Ask which ones are cleared by the kidneys and what dose is safe for your kidney function.
- Don’t take NSAIDs without checking your eGFR. Even one dose can cause acute kidney injury in seniors.
- Keep a copy of your eGFR and drug list in your wallet or phone. Bring it to every appointment.
The goal isn’t to find the perfect number. It’s to avoid the worst mistake: giving a drug that builds up because the kidneys can’t clear it. That’s not bad luck. It’s preventable.
The Future Is Personalized
The field is changing. In 2024, a new equation called CKD2024 was introduced-it combines creatinine and cystatin C with age-specific adjustments. Early results show 15% better accuracy in patients over 80. The National Institute on Aging is funding a $4.2 million project called SAGE to build point-of-care tests that adjust for muscle loss and nutrition.But none of that matters if we keep using the same outdated formulas. The real breakthrough isn’t a new equation-it’s a new mindset. Kidney function isn’t a number on a page. It’s a reflection of a person’s body, their muscle, their health, their age. And for seniors, one-size-fits-all doesn’t just fail-it can kill.
Ask the right questions. Demand better tools. And never assume a lab result tells the whole story.
What’s the best way to estimate kidney function in seniors?
For seniors over 75, especially those who are frail, underweight, or have low muscle mass, the BIS1 or FAS equations are more accurate than standard ones like CKD-EPI. For those with obesity or normal muscle mass, Cockcroft-Gault using ideal body weight works better. Cystatin C testing adds clarity when creatinine results are misleading. No single method is perfect-choose based on the individual’s body type and health status.
Why is creatinine misleading in older adults?
Creatinine is a waste product from muscle breakdown. As people age, they naturally lose muscle-even if they don’t look thin. A senior with low muscle mass may have normal creatinine levels, but their kidneys could be failing. This makes creatinine-based estimates like eGFR falsely reassuring. That’s why cystatin C or muscle-adjusted equations like BIS1 are needed.
Which medications are most dangerous if kidney function is misestimated?
Drugs cleared by the kidneys include anticoagulants (dabigatran, rivaroxaban), diabetes meds (metformin), pain relievers (NSAIDs), antibiotics (vancomycin, aminoglycosides), and heart drugs (digoxin, amiodarone). Even small dosing errors can lead to bleeding, confusion, kidney failure, or death in seniors. Always check if your meds need kidney-based adjustments.
Can I trust the eGFR number from my doctor’s computer?
Not always. Most electronic health records use CKD-EPI by default, which overestimates kidney function in frail seniors. Ask your doctor which equation was used. If you’re over 75 or underweight, request BIS1 or cystatin C testing. Many pharmacists now override EHR defaults weekly to prevent errors.
Should I stop taking NSAIDs if I’m over 65?
Yes, if your eGFR is below 60 mL/min/1.73m². Even occasional use of ibuprofen or naproxen can cause sudden kidney injury in older adults. Acetaminophen is safer for pain relief. If you’re taking NSAIDs regularly, ask your doctor to check your kidney function first-and consider alternatives.
Karandeep Singh
December 1, 2025 AT 06:26creatine levels mean nothing for old folks
Debbie Naquin
December 2, 2025 AT 10:01The reliance on CKD-EPI in clinical practice is a structural failure of evidence translation. The equation’s bias toward muscle mass as a proxy for glomerular filtration is ontologically flawed in aging populations-where sarcopenia decouples biomarker integrity from physiological function. We’re not just misestimating GFR-we’re misrepresenting renal physiology through a young-adult lens. BIS1 and cystatin C aren’t ‘alternatives’-they’re corrections to a broken paradigm.
Suzanne Mollaneda Padin
December 3, 2025 AT 20:47I work in a geriatric clinic and we switched to BIS1 for everyone over 75 two years ago. The drop in adverse drug events was immediate. One patient on rivaroxaban had her dose cut in half after cystatin C came back low-her creatinine was ‘normal’. She’s been stable since. Don’t trust the EHR. Trust the patient’s frailty.
Bonnie Youn
December 4, 2025 AT 15:17Stop letting computers decide who lives and who dies. If your grandma is thin and tired and her creatinine is ‘fine’-she’s not fine. Ask for cystatin C. Demand it. Your doctor might not know-but you do. And that’s power. 💪
James Allen
December 5, 2025 AT 07:01Let’s be real-this is just another liberal healthcare overcomplication. Back in my day, we used creatinine and lived. Now we need five tests and a PhD to prescribe a pill? The EHR isn’t the problem-the problem is overmedicating old people to begin with. Maybe we should stop giving them so many drugs instead of making the math harder.
Alexander Williams
December 5, 2025 AT 12:09CKD-EPI’s performance degradation in elderly populations is a well-documented artifact of its normalization assumptions. The inclusion of race in earlier iterations compounded systemic bias, but even the race-free variant remains statistically biased against low-muscle phenotypes. BIS1’s incorporation of age-sex-creatinine interaction terms provides a more robust multivariate estimate, though its adoption is hindered by EHR vendor inertia and lack of CPT coding.
Amber-Lynn Quinata
December 5, 2025 AT 18:26My mom was hospitalized because her doctor trusted the computer. She’s 82, weighs 98 lbs, and they gave her the same dose of metformin as a 50-year-old man. She ended up in lactic acidosis. I had to fight for three weeks to get them to listen. Now I print out the NKF calculator every time we go in. They roll their eyes. But she’s alive. 🙏
elizabeth muzichuk
December 6, 2025 AT 03:00This is why I don’t trust the medical system. They don’t care about us old people. They just want to push pills and get paid. Cystatin C? BIS1? They don’t want to pay for it. They’d rather kill us quietly with a wrong dose. This isn’t medicine-it’s corporate negligence wrapped in white coats.
Lauryn Smith
December 7, 2025 AT 02:29I’m a nurse and I’ve seen this too many times. A patient’s creatinine looks fine, but they’re confused, falling, swollen. We check cystatin C-and boom, kidney function is half of what the system says. I always tell families: if something feels off, ask for the test. You’re not being difficult. You’re saving their life.
amit kuamr
December 7, 2025 AT 19:55Why bother with all these equations when most seniors are on 10 meds anyway? The real problem is polypharmacy not kidney math. Fix the prescribing culture not the calculator
ariel nicholas
December 8, 2025 AT 21:39Let’s not pretend this is about science-it’s about control. The pharmaceutical industry funds the EHRs, the EHRs push CKD-EPI, the doctors click ‘accept’, and the patients get overdosed. Meanwhile, BIS1? It’s free. It’s accurate. But it’s not in the system because it doesn’t make money. This isn’t medicine. It’s a rigged game.
Mary Ngo
December 9, 2025 AT 10:14It is a known fact that the medical establishment has been systematically suppressing the use of cystatin C and BIS1 due to financial interests tied to the entrenched CKD-EPI algorithm and its integration into proprietary EHR platforms. The National Kidney Foundation’s 2023 update was a political compromise, not a scientific breakthrough. The true solution lies in decentralized, open-source renal function calculators-free from corporate influence. If you are reading this, you are part of the resistance. Share this. Print it. Demand transparency.