What Is Triple Inhaler Therapy for COPD?
Chronic Obstructive Pulmonary Disease (COPD) isn’t just about feeling winded. For many, it’s repeated flare-ups-called exacerbations-that send them to the hospital, disrupt sleep, and make everyday tasks like climbing stairs feel impossible. Triple inhaler therapy combines three medications in one device: a long-acting muscarinic antagonist (LAMA), a long-acting beta-agonist (LABA), and an inhaled corticosteroid (ICS). Together, they tackle airway narrowing, inflammation, and mucus buildup at the same time. This isn’t a new idea, but the way it’s being used today is more precise than ever.
Before triple therapy, most patients were on dual inhalers-either LAMA/LABA or LABA/ICS. But for those with frequent flare-ups and high blood eosinophil levels (300 cells/µL or more), studies showed they still got sick often. That’s where triple therapy steps in. The 2024 GOLD guidelines updated their stance: triple inhalers are no longer a default option. They’re a targeted tool for a specific group.
Who Actually Benefits from Triple Therapy?
Not everyone with COPD needs three drugs. In fact, using triple therapy when it’s not needed can do more harm than good. The key is identifying the right patients. If you’ve had two or more moderate flare-ups in the past year-or one severe one that landed you in the hospital-and your blood test shows eosinophils at 300 or higher, triple therapy has been shown to cut exacerbations by about 25% compared to dual bronchodilators alone.
But here’s the catch: if your eosinophil count is below 100, triple therapy offers almost no benefit. Worse, it raises your risk of pneumonia. Studies show fluticasone-based triple inhalers increase pneumonia risk by nearly 83% compared to budesonide-based ones. That’s why doctors now check your eosinophil count before prescribing. It’s not a guess. It’s a measurement.
Real-world data from the UK tracked over 31,000 COPD patients. When researchers adjusted for the fact that many were taken off ICS before switching to dual therapy, the supposed advantage of triple inhalers disappeared. That means the benefit isn’t just from adding a third drug-it’s from stopping an ineffective one and starting the right one for your body.
Single Inhaler vs. Multiple Inhalers: The Adherence Factor
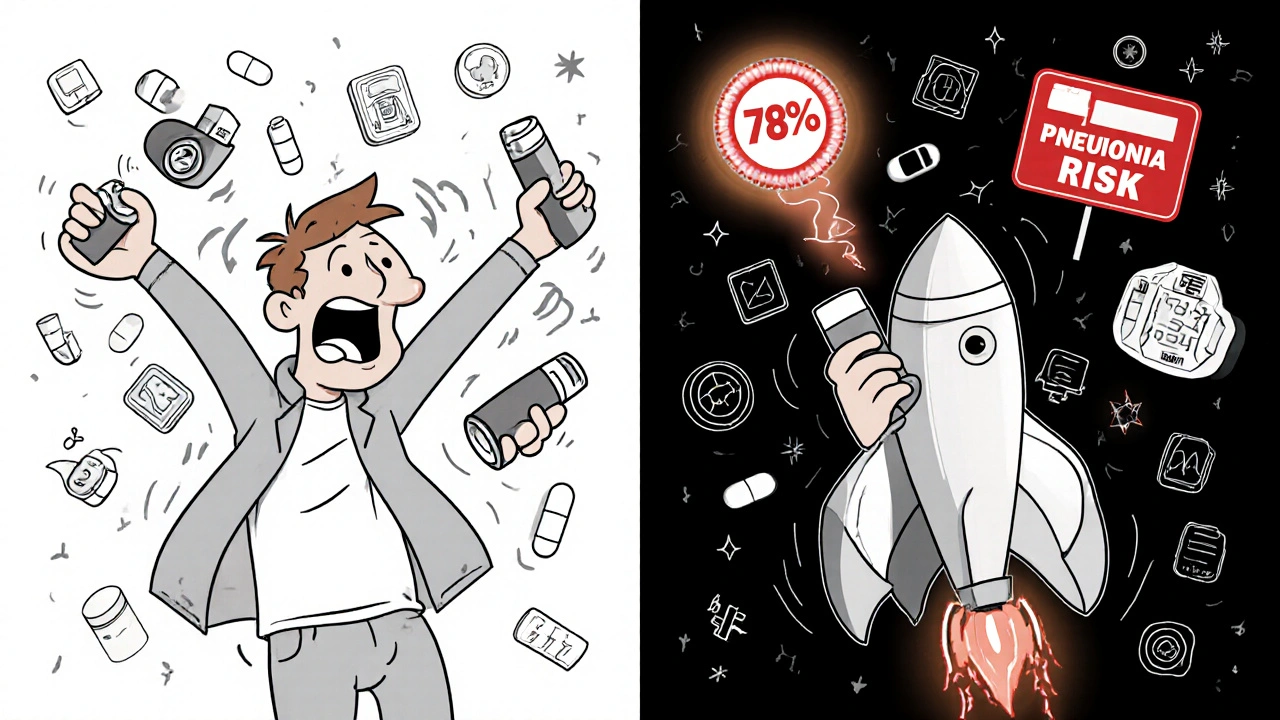
Even the best medicine won’t help if you don’t take it. Triple therapy comes in two forms: multiple-inhaler (MITT) and single-inhaler (SITT). MITT means carrying and using three separate devices-sometimes up to four puffs a day. SITT, like Trelegy Ellipta or Trimbow, delivers all three drugs in one puff, once daily.
Adherence rates tell the story. In the TARGET study, 78% of patients on SITT took their medication correctly after 12 months. For MITT users? Only 62%. Why? Simple: forgetting doses, mixing up inhalers, or feeling overwhelmed by the routine. One patient told researchers, “I had three inhalers in my bag. I’d leave one at work, forget which one was which, and end up skipping days.”
When patients switched from MITT to SITT, their exacerbations dropped by 37% in just six months. The reason? Not because the medicine changed-because they actually took it.
Which Triple Inhaler Is Right for You?
Not all triple inhalers are the same. Three main brands dominate the market:
- Trelegy Ellipta (fluticasone furoate/umeclidinium/vilanterol): One puff daily. Delivers 100/62.5/25 mcg. Higher pneumonia risk, especially in older adults.
- Trimbow (budesonide/glycopyrronium/formoterol): Two puffs twice daily. Extrafine particles penetrate deeper into the lungs. Lower pneumonia risk than fluticasone.
- QBreva (beclomethasone/glycopyrronium/formoterol): Also twice daily, similar to Trimbow. Less widely available in the U.S.
Particle size matters. Extrafine formulations like Trimbow reach smaller airways more effectively, which may explain why they show better symptom control in some studies. But the biggest difference isn’t the drug-it’s the dosing schedule. Once-daily Trelegy improves adherence, but twice-daily Trimbow may offer better lung delivery. Your doctor will weigh your lifestyle, lung function, and risk of pneumonia to choose.
The Pneumonia Risk You Can’t Ignore
Every triple inhaler with an inhaled corticosteroid carries a warning: increased pneumonia risk. The FDA requires a black box warning on these products. Why? Because steroids suppress local immune responses in the lungs. In patients with low eosinophils, this suppression offers no benefit-but still leaves them vulnerable.
One study found patients on fluticasone-based triple therapy had 1.83 times the risk of pneumonia compared to those on budesonide. That’s not a small difference. It’s life-threatening. That’s why guidelines now say: if your eosinophils are below 100, don’t start triple therapy. If you’re already on it and your counts drop, reconsider.
Signs of pneumonia? Fever, new or worsening cough, thick yellow or green mucus, chest pain when breathing, or sudden shortness of breath. If you’re on triple therapy and feel this way, call your doctor immediately. Don’t wait. Don’t assume it’s just a COPD flare.
Cost, Access, and the Hidden Barrier
Trelegy Ellipta costs $75 to $150 a month out-of-pocket in the U.S. For Medicare beneficiaries on fixed incomes, that’s a hard choice: pay for medicine or pay for groceries. A 2022 study found 22.3% of Medicare patients skipped doses because of cost. That’s not noncompliance-it’s survival.
Some insurers require prior authorization. Others only cover it after you’ve tried dual therapy first. And even when covered, pharmacy stock issues can delay refills. One patient reported going three weeks without her inhaler because the pharmacy couldn’t get it in. She ended up in the ER with a severe exacerbation.
Solutions? Ask your doctor about patient assistance programs. Many manufacturers offer copay cards that drop the monthly cost to under $10. Some pharmacies offer medication synchronization-getting all your prescriptions on the same refill schedule-to reduce missed doses.

How Doctors Decide: Biomarkers and Beyond
Doctors aren’t guessing anymore. They’re using data. Blood eosinophil count is the gold standard. But it’s not perfect. Eosinophils can dip after an infection or steroid use. That’s why some clinics now test twice-once at diagnosis, once before starting therapy.
Research is moving fast. The EXACT study is testing fractional exhaled nitric oxide (FeNO), a breath test that measures airway inflammation. Early results suggest it might predict ICS response better than eosinophils in some patients. By 2027, experts predict biomarker-guided therapy will be standard for all advanced COPD cases.
But here’s the reality: even with perfect testing, 80% of COPD patients still don’t qualify for triple therapy. Most do better with LAMA/LABA alone. The goal isn’t to treat everyone with three drugs. It’s to treat the right people with the right drugs-and avoid the ones who don’t need it.
What Happens If It Doesn’t Work?
Not every patient responds. Sometimes, it’s not the medicine-it’s the technique. Studies show 50-70% of people who seem to “fail” triple therapy are actually using the inhaler wrong. The Ellipta device requires a deep, forceful inhale. If you just puff gently, the medicine hits your throat, not your lungs.
Doctors now use checklists to verify technique. You’ll be asked to demonstrate your inhaler use at every visit. If you’re still having flare-ups after three months, your doctor will check your technique, your adherence, your eosinophil levels, and whether you’re smoking or exposed to air pollution.
If triple therapy isn’t working, alternatives exist. New biologics like dupilumab (used for asthma and eczema) are being tested in COPD patients with high eosinophils. Early results from the LIBERTY POSEIDON trial show promise in reducing exacerbations without the pneumonia risk of steroids.
The Bottom Line: Precision, Not Power
Triple inhaler therapy isn’t a magic bullet. It’s not for everyone. But for the right person-someone with frequent flare-ups and high eosinophils-it can mean the difference between staying home and ending up in the hospital. The key is precision: test first, choose wisely, monitor closely.
Don’t let marketing or pressure from well-meaning friends push you into a treatment you don’t need. And if you’re already on it, ask your doctor: “Is this still right for me?” Your lungs will thank you.
David Cunningham
November 23, 2025 AT 14:57Holly Schumacher
November 24, 2025 AT 11:43Daniel Jean-Baptiste
November 24, 2025 AT 21:39New Yorkers
November 26, 2025 AT 06:09Danny Nicholls
November 27, 2025 AT 00:43Rahul Kanakarajan
November 27, 2025 AT 21:59luke young
November 29, 2025 AT 01:06james lucas
November 29, 2025 AT 13:23Jessica Correa
December 1, 2025 AT 04:14manish chaturvedi
December 1, 2025 AT 04:37Michael Fitzpatrick
December 2, 2025 AT 03:26Shawn Daughhetee
December 3, 2025 AT 13:44