CYP2D6 Risk Calculator
Assess Your Codeine Risk
Based on FDA data and genetic research, this calculator estimates your risk of severe reaction to codeine based on ancestry and age.
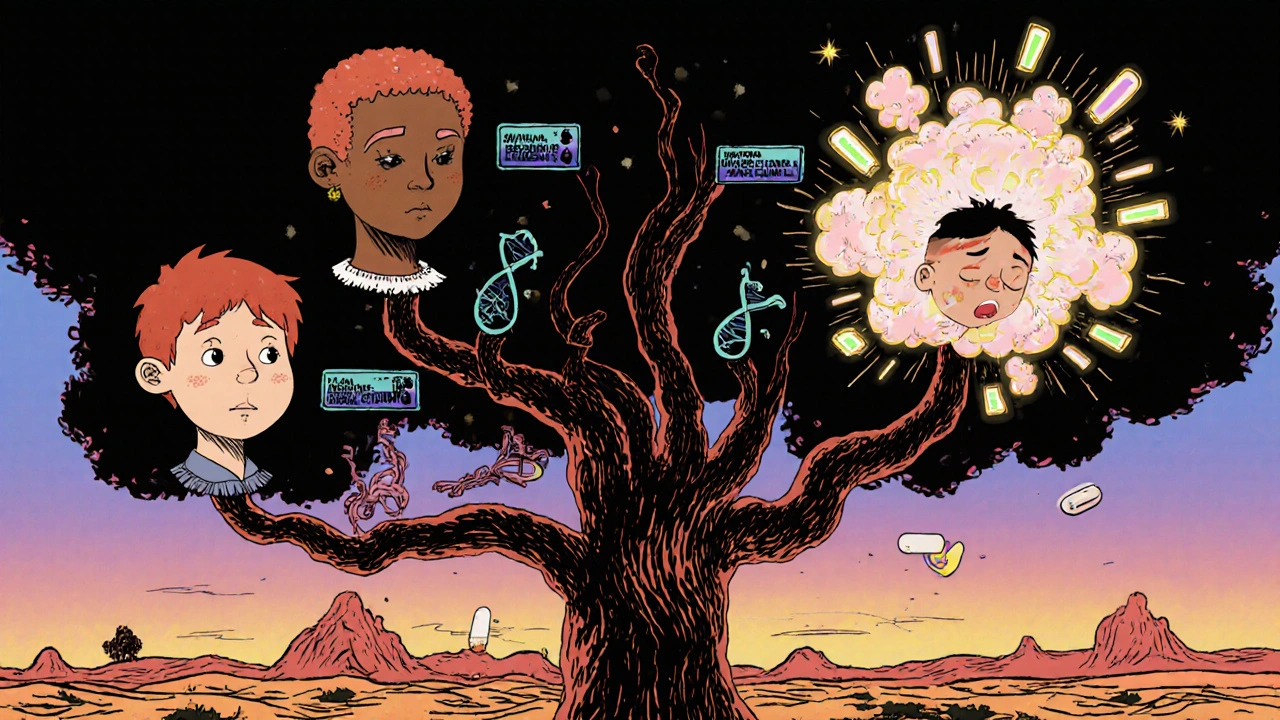
Most people think of codeine as a safe, mild painkiller - something you take after a dental procedure or for a stubborn cough. But for a small group of people, even one pill can be deadly. It’s not because they took too much. It’s because their body turns codeine into morphine too fast. This isn’t rare. It’s genetic. And if you don’t know about it, you could be at serious risk.
How Codeine Turns Into a Deadly Substance
Codeine itself doesn’t relieve pain. It’s just a placeholder. Your body has to convert it into morphine - the real painkiller - using an enzyme called CYP2D6. For most people, this process works slowly and steadily. But for about 1 to 7% of the population, depending on ancestry, this enzyme is hyperactive. These people are called CYP2D6 ultrarapid metabolizers.
They have extra copies of the CYP2D6 gene. That means their liver turns codeine into morphine up to 4.5 times faster than normal. Within hours, morphine levels in their blood can spike far beyond what’s safe. The result? Respiratory depression - slow, shallow breathing that can stop entirely. That’s how otherwise healthy adults and children have died after taking a standard dose of codeine.
The U.S. Food and Drug Administration (FDA) looked at 64 cases of serious harm linked to codeine. Twenty-four of those were fatal. Twenty-one of the deaths were in children under 12. In 15 of the cases where blood levels were tested, 13 had morphine levels above the toxic range. And in the 10 cases where genetic testing was done, seven were ultrarapid metabolizers. Five of those seven died.
Who’s at Risk?
This isn’t random. It’s tied to genetics - and ancestry. In European populations, about 3% are ultrarapid metabolizers. In North African and Ethiopian populations, that number jumps to nearly 30%. In East Asians, it’s closer to 1-2%. That means someone from Ethiopia or Morocco taking codeine for a headache might be at 15 times higher risk than someone from Japan.
Children are especially vulnerable. Their bodies are smaller, and their metabolism is still developing. After the FDA issued its warning in 2013, codeine prescriptions for kids under 12 dropped by half in the U.S. The American Academy of Pediatrics now says codeine should never be used after tonsillectomy or adenoidectomy - exactly the surgeries where it was once routinely given for pain. One case in the New England Journal of Medicine described a 15-month-old child who died after a routine surgery. Post-mortem tests showed they were an ultrarapid metabolizer. The morphine level in their blood was lethal.
But it’s not just kids. Adults can die too. A 2023 study in Nature found that ultrarapid metabolizers were more likely to develop Codeine Use Disorder - not because they were addicted, but because they felt the high from morphine so intensely and quickly. That’s the same mechanism that leads to overdose: too much morphine, too fast.
The FDA Warning and What Changed
In September 2013, the FDA didn’t just issue a warning - they forced drugmakers to put a boxed warning on every codeine product. That’s the strongest type of warning they can give. It says clearly: “Respiratory depression and death have occurred in children who received codeine after tonsillectomy or adenoidectomy and had evidence of being CYP2D6 ultrarapid metabolizers.”
Europe followed. New Zealand’s Medsafe issued similar alerts. By 2015, the European Medicines Agency banned codeine for children under 12 entirely. In hospitals and clinics across the U.S. and Europe, doctors stopped prescribing it for kids. Many stopped prescribing it for adults too.
But here’s the problem: not every doctor knows about this. Not every pharmacy checks. And unless you’ve had genetic testing, you might never know you’re at risk. The symptoms of morphine toxicity - extreme drowsiness, difficulty waking up, slow breathing, nausea - can look like just a bad reaction to pain meds. They’re not always recognized as a genetic emergency.
What Should You Take Instead?
If you’re an ultrarapid metabolizer, codeine is dangerous. So is tramadol - another drug that turns into a potent opioid through CYP2D6. But you don’t have to go without pain relief.
The Clinical Pharmacogenetics Implementation Consortium (CPIC) says clearly: avoid codeine and tramadol if you’re an ultrarapid metabolizer. Instead, use opioids that don’t rely on CYP2D6. Morphine, hydromorphone, and fentanyl are safe alternatives because they’re active as-is. No conversion needed. Non-opioid options like acetaminophen or ibuprofen are also effective for mild to moderate pain.
For chronic pain, some doctors now recommend oxycodone or hydrocodone. But be careful - these drugs are partially metabolized by CYP2D6 too. While they’re safer than codeine, they still carry some risk for ultrarapid metabolizers. That’s why CPIC recommends sticking to morphine or fentanyl when possible.

Can You Get Tested?
Yes. Genetic tests for CYP2D6 are available. They’re not cheap - $200 to $500 - and insurance often requires prior approval. Results take 3 to 14 days. But if you’ve had an unexpected reaction to codeine, or if a close family member had a bad reaction, testing could save your life.
Some hospitals in the U.S. and Europe now offer pre-emptive pharmacogenetic testing as part of routine care. Vanderbilt University is running a $2.5 million NIH-funded study to develop rapid CYP2D6 tests that give results in under two hours. That could change everything - especially in emergency rooms or before surgery.
Right now, only about 15-20% of major U.S. medical centers do routine testing. But that’s changing. As costs drop and awareness grows, more doctors are asking: “Have you ever had a bad reaction to codeine?”
What to Do Now
If you’ve been prescribed codeine - especially if you’re of North African, Ethiopian, or European descent - ask your doctor: “Could I be a CYP2D6 ultrarapid metabolizer?”
If you’re planning surgery or have chronic pain, request a non-CYP2D6-dependent painkiller. If you’ve ever felt unusually drowsy or had trouble breathing after taking codeine, get tested. Don’t wait for a tragedy to happen.
This isn’t about avoiding medication. It’s about using the right one. Codeine isn’t evil. It’s just not safe for everyone. Understanding your genes isn’t science fiction - it’s the future of medicine. And right now, it could be the difference between life and death.
Can codeine be fatal even at normal doses?
Yes. For people who are CYP2D6 ultrarapid metabolizers, even a standard dose of codeine can turn into a lethal amount of morphine within hours. The FDA confirmed this with 24 deaths linked to codeine, including 21 children under 12. These weren’t overdoses - they were genetic reactions.
How do I know if I’m an ultrarapid metabolizer?
You can get tested through a simple blood or saliva genetic test. Many labs offer CYP2D6 testing, and results usually take 3-14 days. If you’ve had a bad reaction to codeine, or if a close family member did, testing is strongly recommended. Some hospitals now test routinely before surgery.
Is codeine banned for children?
In the U.S., codeine is not banned, but the FDA strongly warns against its use in children under 12, especially after tonsil or adenoid surgery. In Europe and New Zealand, it’s officially restricted for this age group. Many doctors now avoid prescribing it to children entirely.
Are there safer painkillers than codeine?
Yes. Morphine, hydromorphone, and fentanyl don’t rely on CYP2D6 to work, so they’re safer for ultrarapid metabolizers. Non-opioid options like acetaminophen and ibuprofen are also effective for mild to moderate pain. Avoid tramadol too - it’s metabolized the same way as codeine.
Does ethnicity affect my risk?
Yes. About 3-7% of Europeans, up to 29% of North Africans and Ethiopians, and 1-2% of East Asians are ultrarapid metabolizers. If you’re from a population with high rates of this gene variant, your risk is significantly higher - even if you’ve never had a reaction before.
Why isn’t everyone tested before taking codeine?
Testing isn’t yet standard practice in most clinics. It’s expensive, takes time, and many doctors aren’t trained in pharmacogenetics. But as costs drop and awareness grows, more hospitals are adopting pre-emptive testing - especially before surgeries or for chronic pain patients.

Aidan McCord-Amasis
November 16, 2025 AT 00:02Katie Baker
November 17, 2025 AT 09:16Hollis Hollywood
November 18, 2025 AT 01:51It’s honestly terrifying how many people are walking around with this genetic time bomb and don’t even know it. I’ve had family members who swore they "never react to meds"-until they took codeine and ended up in the ER with breathing issues. No one connects the dots because it looks like an "accidental overdose"-but it’s not. It’s biology. And the fact that this isn’t routine testing before any opioid prescription is a systemic failure. I get that labs cost money and doctors are overworked, but when you’re talking about kids dying after tonsillectomies, we’re not talking about convenience anymore. We’re talking about basic human safety. The FDA warning was a start, but it’s not enough. Pharmacies should be required to flag high-risk ethnicities on scripts. Hospitals should screen before surgery. Insurance companies should cover testing without a fight. This isn’t sci-fi-it’s 2024. We map genomes before we have babies, but we still let people take codeine like it’s aspirin? That’s not just negligence. It’s negligence with a death toll.
Edward Ward
November 19, 2025 AT 13:52Let’s not forget-tramadol is just as dangerous for ultrarapid metabolizers, and it’s prescribed constantly for "mild" pain. I’ve seen it in my own family: my uncle, a 62-year-old with chronic back pain, was on tramadol for years until he had a near-fatal episode after a flu. Morphine levels spiked. He didn’t know why. No one tested him. Now he’s on hydromorphone, and he’s functional again. But how many others are still suffering-or dying-because their doctor didn’t think to ask about family history or genetic risk? The CPIC guidelines are crystal clear, but most primary care docs don’t even know what CPIC stands for. Pharmacogenomics isn’t a niche field anymore-it’s foundational. We need mandatory CYP2D6 education in med school, not as an elective. And we need it yesterday. This isn’t about "personal responsibility." It’s about the system failing to protect people who didn’t ask to be born with a genetic variant that makes a common drug lethal.
Adam Dille
November 20, 2025 AT 08:41Ogonna Igbo
November 20, 2025 AT 22:05Of course this happens. In Nigeria, codeine is sold in soda shops like it’s candy. People drink it for fun. They call it "syrup." Kids as young as 10 are mixing it with Sprite and coughing it down like it’s a party drink. No one tests for genes here. No one even knows what CYP2D6 means. We’ve got bodies piling up and the government still won’t ban it. Why? Because it’s cheap. Because the pharmaceutical companies don’t care. Because the rich don’t take codeine-they take oxycodone. The poor? They get the poison that kills their children. This isn’t a medical issue-it’s a colonial legacy. You test for genes in Nashville, but in Lagos, they test for dead bodies.
Shyamal Spadoni
November 22, 2025 AT 21:26Wait… this is all a scam. The FDA doesn’t care about you. They want you to buy expensive "safe" opioids instead. Morphine? Fentanyl? Those are controlled substances. Codeine? Cheap. Easy to make. Easy to ban. But if they make you scared of codeine, you’ll take the real killers-prescribed by doctors who get kickbacks. And now you’re hooked on something even more dangerous. They didn’t ban codeine to protect you-they did it to sell you something else. They’re using genetics as a cover. Look at the data: deaths dropped after the ban… but opioid overdoses skyrocketed. Coincidence? I think not. The real danger isn’t your genes-it’s the system that profits from your fear.
Jessica Chambers
November 23, 2025 AT 18:10Chris Bryan
November 24, 2025 AT 04:02This is why America is falling apart. We let genetics dictate medicine now? Next thing you know, they’ll tell you not to drink milk if you’re from Europe, or not to eat rice if you’re Asian. This isn’t medicine-it’s eugenics with a lab coat. They’re dividing us by DNA to control what we take. And who’s paying for these "tests"? Big Pharma. Who’s pushing the narrative? The same people who profit from fentanyl prescriptions. Don’t be fooled. This isn’t safety. It’s control. And if you’re not careful, they’ll start denying you meds based on your ancestry. Welcome to the future.
BABA SABKA
November 24, 2025 AT 17:32Look, I’m Nigerian. My uncle died on codeine after a dental procedure. No one knew. No one tested. But here’s the thing-this isn’t unique to codeine. The whole pharmacological system is broken. We treat symptoms, not systems. We don’t test for CYP2D6 because it’s not profitable. We don’t train doctors because it’s not in the curriculum. We don’t educate patients because it’s too complicated. But here’s the real issue: we’re treating medicine like a one-size-fits-all factory. And people are the broken parts. The solution isn’t just testing. It’s rebuilding the entire model. Personalized medicine isn’t a luxury-it’s the only ethical way forward. Stop treating genetics like a side note. It’s the core.
John Foster
November 26, 2025 AT 13:37There’s a deeper metaphysical truth here, and it’s not in the genes-it’s in the silence. We live in an age of hyper-optimization, where every molecule is quantified, every enzyme mapped, every SNP cataloged-and yet, we still allow a child to die from a pill because no one asked the right question. The tragedy isn’t the mutation. The tragedy is the assumption. The assumption that the body is a machine that behaves uniformly. The assumption that pain is universal. The assumption that medicine is neutral. But it’s not. Medicine is a mirror. It reflects our biases, our laziness, our fear of complexity. We don’t test for CYP2D6 because we don’t want to confront the fact that biology doesn’t care about our protocols. It doesn’t care about our guidelines. It doesn’t care about our convenience. It just is. And in that is, we are forced to acknowledge that we are not the masters of our own bodies. We are guests. And we have been rude. The codeine death isn’t a failure of pharmacology. It’s a failure of humility.
Andrew Eppich
November 26, 2025 AT 18:23