Antidepressant Tapering Calculator
How to Use This Tool
Select your antidepressant, duration of use, and current dose to calculate a safe tapering schedule. Always consult your healthcare provider before making changes to your medication.
Your Tapering Schedule
Estimated taper duration:
Taper Steps
Key Warnings
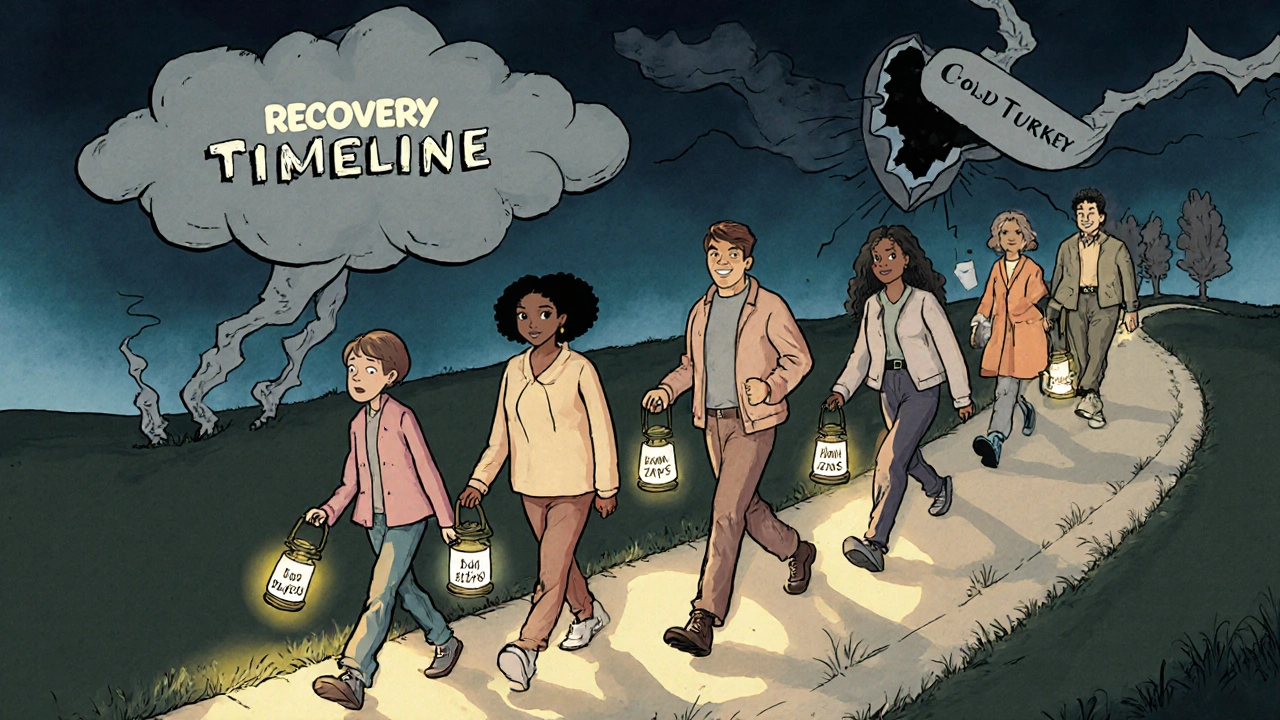
Never stop cold turkey. Abrupt discontinuation can cause severe withdrawal symptoms.
For short half-life drugs (Paroxetine, Venlafaxine): Taper over 8-12 weeks or longer. These medications have the highest withdrawal risk.
For long half-life drugs (Fluoxetine): You may be able to taper faster, but still do so gradually.
Do not skip doses of short-acting antidepressants. Missing even one dose can trigger symptoms.
Track your symptoms during the taper. If symptoms worsen, contact your prescriber immediately.
Stopping antidepressants isn’t as simple as just skipping a pill. For many people, it triggers a wave of physical and emotional symptoms that feel terrifyingly real - dizziness, electric shock sensations in the head, nausea, insomnia, and overwhelming anxiety. These aren’t signs of relapse. They’re not weakness. They’re antidepressant discontinuation syndrome, a well-documented physical withdrawal reaction that happens when the brain and body have to readjust after months or years of medication.
Why This Happens
Antidepressants don’t make you addicted in the way drugs like opioids or benzodiazepines do. You won’t crave them or use them to get high. But your brain changes around them. Over time, it adapts to the presence of the drug - adjusting serotonin, norepinephrine, or other neurotransmitter levels to maintain balance. When you suddenly stop, that balance collapses. Your brain hasn’t had time to rebuild its natural production and regulation systems. That’s when symptoms kick in. This isn’t a myth or a marketing trick. It’s a biological reality. The term "discontinuation syndrome" was coined by pharmaceutical companies to avoid the stigma of "withdrawal," but experts like Dr. David Healy and clinical guidelines from the American Academy of Family Physicians agree: this is a classical withdrawal syndrome. The body has adapted. And when you remove the drug, it reacts.The Symptoms: What to Watch For
Symptoms usually show up within 2 to 4 days after stopping - sometimes within hours if you’re on a short-acting drug like paroxetine or venlafaxine. The classic pattern is remembered by the mnemonic FINISH:- Flu-like symptoms: fatigue, muscle aches, chills, headaches, diarrhea
- Insomnia: trouble falling or staying asleep, vivid or disturbing dreams
- Nausea: feeling sick to your stomach, sometimes vomiting
- Ibalance: dizziness, vertigo, unsteady gait, feeling off-balance
- Sensory disturbances: "brain zaps" - sudden, brief electric shock feelings in the head, often triggered by eye movement; tingling, numbness, or buzzing sensations
- Hyperarousal: anxiety, agitation, irritability, panic attacks, restlessness
Which Antidepressants Cause the Worst Withdrawal?
Not all antidepressants are equal when it comes to withdrawal. The biggest factor is half-life - how long the drug stays in your system.- Short half-life drugs (highest risk): Paroxetine (Paxil), venlafaxine (Effexor), and fluvoxamine. These leave your body fast, so symptoms hit hard and fast. Up to 47% of venlafaxine users report severe withdrawal. Paroxetine is especially notorious for brain zaps and nausea.
- Long half-life drugs (lower risk): Fluoxetine (Prozac). It stays in your system for days, acting like a slow taper. People switching from paroxetine to fluoxetine often find relief.
- Tricyclics (TCAs): Like amitriptyline or nortriptyline. Withdrawal can include tremors, stiff muscles, and movement problems that mimic Parkinson’s.
- MAOIs: The most dangerous to stop abruptly. Can cause severe agitation, psychosis, catatonia, or myoclonus (involuntary muscle jerks). Requires immediate medical supervision.

How Long Does It Last?
Most guidelines say symptoms last 1-2 weeks. But real-world experience tells a different story. The NHS and Mayo Clinic say symptoms resolve quickly with medication restart. That’s true - if you take the original drug again, symptoms often vanish within 72 hours. But for many, the problem doesn’t stop there. Patient communities like Surviving Antidepressants, with over 15,000 members, report that 73% of people experience symptoms longer than two weeks. Nearly 30% say symptoms lasted six months or more. A 2022 study in the Journal of Clinical Psychiatry found 18.7% of SSRI users had symptoms beyond three months. This isn’t rare. It’s underreported. Doctors often dismiss these cases as "relapse" or "anxiety." But relapse takes weeks to develop. Discontinuation symptoms appear within days. And they respond to reinstatement - not new therapy or higher doses.How to Stop Safely: The Right Way to Taper
The single most effective way to avoid severe withdrawal? Don’t stop cold turkey. Taper slowly.- For most SSRIs: taper over at least 4-6 weeks. For paroxetine or fluvoxamine, aim for 8 weeks.
- For venlafaxine: 8-12 weeks is standard. Some people need even longer.
- For fluoxetine: you may be able to stop faster due to its long half-life, but still taper gradually.
What to Do If Symptoms Hit
If you’ve stopped and symptoms start:- Don’t panic. This is temporary - even if it feels endless.
- Contact your prescriber immediately. Reintroducing the original medication - even a small dose - usually stops symptoms within 1-3 days.
- If you can’t reach your doctor, consider a temporary return to the lowest dose you were on. Don’t wait for symptoms to worsen.
- Track your symptoms. Write down what you feel, when it started, and how intense it is. This helps your doctor distinguish withdrawal from relapse.
High-Risk Situations to Watch For
Some moments are especially dangerous for stopping antidepressants:- Pregnancy: 41% of pregnant women stop antidepressants without medical advice. But sudden withdrawal can harm both mother and baby. Always work with a psychiatrist who specializes in perinatal care.
- Switching medications: Going from one antidepressant to another? There should be a washout period and a taper. Never overlap or switch cold turkey.
- Generic switches: If your pharmacy changes your prescription without telling you, you might be getting a different formulation. Ask if it’s bioequivalent.
- Missed doses: Skipping even one dose of a short-acting drug can trigger symptoms. Set phone reminders.
When to Seek Emergency Help
Most withdrawal symptoms are uncomfortable but not dangerous. But if you experience:- Severe confusion or hallucinations
- Extreme agitation or violent thoughts
- Seizures
- Difficulty breathing or chest pain
What You Should Know Before You Start
If you’re considering stopping antidepressants:- Never do it on your own. Even if you feel fine, your brain isn’t.
- Ask your doctor about your drug’s half-life and what a safe taper looks like for you.
- Know your symptoms. Write them down before you start.
- Build a support system. Tell someone you trust what you’re doing.
- Be patient. Healing your nervous system takes time. Rushing it can set you back months.
Can antidepressant withdrawal feel like depression returning?
Yes, it can. Symptoms like low mood, fatigue, and lack of motivation overlap with depression. But timing is the key difference. Withdrawal symptoms start within days of stopping, while relapse takes weeks to develop. If symptoms improve within 72 hours after restarting the medication, it’s withdrawal - not relapse.
Are brain zaps dangerous?
No, brain zaps aren’t dangerous. They’re brief, electric-like sensations in the head, often triggered by eye movement. They’re a hallmark of serotonin discontinuation and usually fade over time. While they’re startling and uncomfortable, they don’t cause brain damage or seizures. Reducing stress, staying hydrated, and tapering slowly can lessen their intensity.
How long should I taper off my antidepressant?
It depends on the drug and how long you’ve taken it. For SSRIs like sertraline or escitalopram, 4-8 weeks is typical. For venlafaxine or paroxetine, aim for 8-12 weeks or longer. If you’ve been on the medication for years, some experts recommend tapering over 6 months. The slower the taper, the lower the risk of severe symptoms.
Can I switch to a different antidepressant to avoid withdrawal?
Sometimes, yes. Switching to fluoxetine (Prozac) - which has a very long half-life - can help smooth the transition off a shorter-acting drug like paroxetine. This is called a "cross-taper." But it must be done under medical supervision. Never switch cold turkey. You risk triggering withdrawal from the first drug and side effects from the new one.
Is it safe to stop antidepressants during pregnancy?
It’s not about safety - it’s about risk balance. Stopping abruptly can trigger withdrawal in the mother and stress the baby. Continuing may carry small risks to fetal development. The decision should be made with a psychiatrist and obstetrician who specialize in perinatal mental health. Never stop without guidance. Many women successfully taper slowly during pregnancy under medical care.

Mark Kahn
November 21, 2025 AT 21:18Hey, just wanted to say this post saved my life. I thought I was going crazy when the brain zaps hit after quitting sertraline. Turned out I wasn't relapsing-I was just withdrawing. Tapering slow with my doc's help made all the difference. You're not alone.
Anne Nylander
November 22, 2025 AT 07:13THIS. SO THIS. I thought i was losing my mind. brain zaps are REAL. dont let anyone tell you its just anxiety. you got this.
Franck Emma
November 22, 2025 AT 20:24So now we're calling it 'discontinuation syndrome' to make pharma look less evil? Cute.
Noah Fitzsimmons
November 24, 2025 AT 19:22Oh wow, someone actually read the entire 2000-word post? Congrats, you're the first person I've seen do that. I'm impressed. Or maybe just bored.
Eliza Oakes
November 24, 2025 AT 21:43Wait, so you're saying antidepressants aren't magic happiness pills? Shocking. Next you'll tell me sugar causes inflammation.
Pravin Manani
November 26, 2025 AT 06:23The pharmacokinetic variability between generic formulations is a critical yet under-addressed issue in clinical practice. The bioequivalence thresholds established by the FDA (80-125% AUC and Cmax) are statistically permissible but clinically insufficient for neuroactive agents with narrow therapeutic windows. This creates a latent discontinuity in receptor occupancy, triggering neuroadaptive destabilization-particularly in patients with prolonged exposure to SSRIs/SNRIs with short half-lives. The phenomenon is not psychological; it is a quantifiable neurochemical recalibration event.
Leo Tamisch
November 26, 2025 AT 10:23Of course it's withdrawal. The pharmaceutical-industrial complex just needed a new term to avoid the moral panic of 'addiction.' 🤓
Also, I once took a 10mg dose of Prozac and felt like I was in a David Lynch film. So yeah. I know.
Daisy L
November 27, 2025 AT 09:20AMERICA NEEDS TO STOP TREATING MENTAL HEALTH LIKE A COSMETIC OPTION!! THIS IS MEDICAL, NOT A CHOICE!! WHY ARE DOCTORS STILL LETTING PEOPLE QUIT COLD TURKEY?!?!?!!??!?!?!
Corra Hathaway
November 28, 2025 AT 02:54You guys are doing amazing!! 💪✨ I know it feels like your brain is melting, but you're not broken-you're healing. And hey, if you need someone to vent to, I'm here. Coffee on me (virtually, of course). ☕❤️
Shawn Sakura
November 28, 2025 AT 18:42thank you for this. i was so scared when i started tapering. my doctor said 'just cut in half' but i found out my pills werent even scored. i ended up using a compounding pharmacy. it was expensive but worth it. you are not alone. 🙏
Paula Jane Butterfield
November 29, 2025 AT 01:19As someone who's helped patients through this for over a decade, I can't stress enough: the 'FINISH' mnemonic is spot-on. But I always add 'C' for 'Cotton Wool'-that's the one no one talks about. It feels like your thoughts are wrapped in bubble wrap. It's terrifying, but temporary. And yes, it's not depression. It's your neurons relearning how to walk.
Simone Wood
November 29, 2025 AT 22:33My GP told me to just 'tough it out' when I stopped citalopram. I ended up in A&E with vertigo and panic attacks. Now I'm on fluoxetine because I'm too scared to try again. Why is this so poorly understood? It's not rocket science.
Swati Jain
December 1, 2025 AT 09:13India has zero guidelines for tapering. I had to read this entire post and print it to show my doctor. He laughed. Said 'you're overthinking.' So I quit cold turkey. Now I have brain zaps every time I sneeze. 🤦♀️
Chris Vere
December 2, 2025 AT 01:50There's a deeper truth here that doesn't get discussed enough. We treat mental health as if it's a switch-on or off. But the brain is not a lightbulb. It's a forest. You don't cut down a tree and expect the ecosystem to instantly rebalance. The body remembers. The nervous system holds memory. What we call 'withdrawal' is just the system trying to remember how to be itself again. And that takes time. And patience. And sometimes, just letting go of the need to fix it immediately.
Clifford Temple
December 3, 2025 AT 21:15THIS IS WHY AMERICA IS WEAK. YOU PEOPLE CAN'T EVEN QUIT A PILLS WITHOUT CRYING? WE USED TO JUST POWER THROUGH IN MY DAY. YOU'RE ALL SOFT.