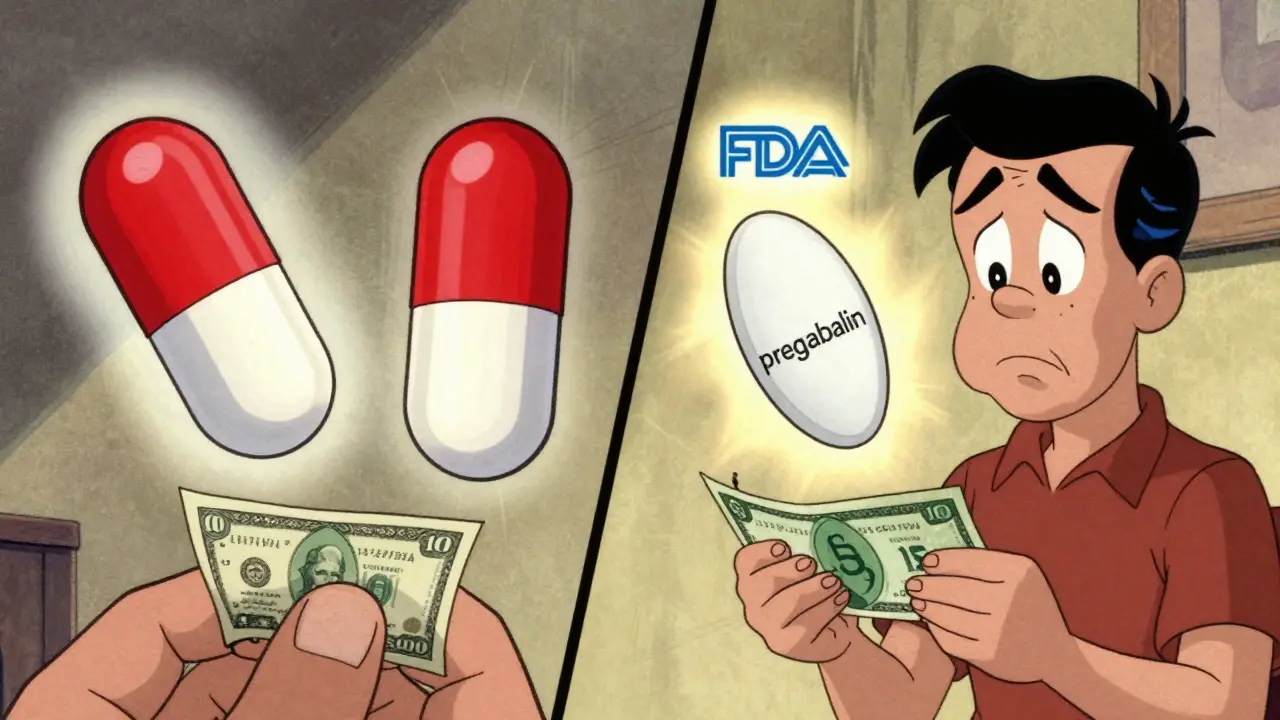
When you pick up a prescription, you might see two names on the label: one you recognize, like Lyrica, and another you don’t, like pregabalin. One costs $300. The other, $15. You might wonder: is the cheaper one really the same? Are you getting less medicine for less money? Or worse-could it be less effective?
The short answer is yes, they’re the same. But the full story matters.
What Exactly Is the Active Ingredient?
Every pill, capsule, or injection has two kinds of ingredients: active and inactive. The active ingredient is what actually treats your condition. It’s the chemical that lowers your blood pressure, balances your thyroid, or eases your depression. The rest? Fillers, dyes, binders, and coatings. They help the pill hold its shape, dissolve properly, or look different-but they don’t do anything medically.
Here’s the rule: if a generic drug is approved by the FDA, it must contain the exact same active ingredient, in the same amount, and in the same form as the brand-name version. That means if your brand-name drug has 10 mg of amlodipine, the generic has 10 mg of amlodipine. No more. No less. And it has to get into your bloodstream at the same rate and to the same level.
How Do We Know Generics Work the Same?
The FDA doesn’t just take a manufacturer’s word for it. They require a test called bioequivalence. This means the generic drug must deliver the active ingredient into your blood within a very tight range-80% to 125%-of what the brand-name drug does. That’s not a guess. It’s measured using real data from healthy volunteers who take both versions and have their blood tested over time.
Let’s say you’re taking metformin for diabetes. The brand-name version is Glucophage. The generic is just metformin. In a bioequivalence study, researchers check two things: how high the drug peaks in your blood (Cmax), and how much total drug your body absorbs over time (AUC). If the generic falls within that 80%-125% window for both, it’s approved. And this isn’t rare. The FDA approves 1,000 to 1,200 generic drugs every year.
And it’s not just lab tests. Real-world data backs it up. A 2019 study in JAMA Internal Medicine looked at over 3.5 million patients using generics for diabetes, high blood pressure, epilepsy, and depression. The results? No difference in outcomes. Blood sugar control. Blood pressure numbers. Seizure frequency. Depression scores. All matched the brand-name versions exactly.
Why Are Generics So Much Cheaper?
Brand-name drugs cost a lot because the company that invented them spent years and millions developing the drug, running clinical trials, and getting approval. Once the patent expires-usually after 20 years-their monopoly ends. That’s when other companies can make copies.
Those companies don’t have to repeat the expensive clinical trials. They just need to prove their version behaves the same in the body. That cuts costs dramatically. No marketing campaigns. No patent lawyers. No R&D teams. Just manufacturing.
The result? Generics cost, on average, 85% less. Metformin (generic for Glucophage) runs about $4 for a 30-day supply. Glucophage? Around $350. Amlodipine (generic for Norvasc)? $2. Norvasc? $400. That’s not a discount. That’s a revolution in access.
Over the last decade, generics saved the U.S. healthcare system more than $2.2 trillion. In 2022 alone, they saved $313 billion. That’s money kept in patients’ pockets and out of insurance premiums.
What About the Differences? Color, Shape, Taste?
Yes, generics look different. They might be blue instead of white. Oval instead of round. Smaller. Bigger. That’s because the brand-name company owns the trademark for how their pill looks. The generic maker can’t copy that design. So they make their own.
Some patients notice the change and worry. “This isn’t the same pill,” they think. But the pill’s job isn’t to look familiar. It’s to deliver the active ingredient. And it does.
Still, changes can affect adherence. A 2022 study from Cedars-Sinai found that patients were 28% more likely to keep taking their meds when they could afford the generic-and 15% better clinical outcomes followed. But if a patient sees a new-looking pill and thinks it’s weaker, they might skip doses. That’s why pharmacists are trained to explain the difference. A two-minute conversation can prevent confusion and keep people healthy.

Are There Exceptions? When Should You Be Careful?
Most of the time, generics are identical in effect. But there’s a small group of drugs called narrow therapeutic index (NTI) medications. These are drugs where even a tiny change in blood level can cause problems. Think warfarin (blood thinner), levothyroxine (thyroid hormone), or certain anti-seizure drugs like phenytoin.
For these, doctors sometimes prefer to stick with one version-brand or generic-because switching could mean small shifts in how the drug works. That doesn’t mean generics are unsafe. It means the margin for error is thinner. The FDA still requires these generics to meet the same 80%-125% bioequivalence standard. But in practice, some prescribers choose consistency to avoid any risk.
That said, a 2022 review in The New England Journal of Medicine found no significant difference in outcomes even for NTI drugs when generics were used properly. The key? Stick with one version once you’ve found what works.
Who Makes These Generics? Are They Safe?
Generics aren’t made in some shady basement. They’re made in the same kind of factories as brand-name drugs. The FDA inspects all drug facilities-whether in the U.S., India, or Germany-with the same strict standards. Every plant must follow Current Good Manufacturing Practices (cGMP). The FDA does about 3,500 inspections a year.
Some of the biggest generic makers are Teva, Mylan, and Sandoz. But over 150 companies compete in the U.S. market. That competition keeps prices low.
There have been quality issues. In 2022, the FDA issued import alerts for 12 plants in India and China. That’s less than 0.5% of all manufacturing sites. And when problems are found, the FDA pulls the product. No compromise.
What Do Patients Actually Experience?
Most people don’t notice a difference. A 2023 GoodRx survey of 5,000 patients found 87% reported no change in how the drug worked. But 12% said they noticed something-mostly mild stomach upset, dizziness, or fatigue.
Could that be the inactive ingredients? Possibly. Some people are sensitive to dyes, lactose, or preservatives. If you’ve never had a reaction to the brand-name drug but get a rash or nausea after switching to the generic, talk to your doctor or pharmacist. It’s rare, but it happens.
On Drugs.com, generics average 4.2 out of 5 stars from over 12,500 reviews. Common comments: “Saved me $300 a month,” “Works just as well,” “No side effects.”
One Reddit user wrote: “Switched from Zoloft to generic sertraline. Got terrible stomach cramps. Went back to Zoloft. Problem gone.” Another said: “Switched to generic amlodipine. Blood pressure better than ever. Saved $280 a month.”
It’s not about the drug. It’s about the person.

Can Your Pharmacist Switch Your Prescription Automatically?
In 49 states, yes. Unless your doctor writes “dispense as written” or “no substitution,” your pharmacist can give you the generic version. That’s by law. Insurance companies often require it. Humana reports 92% of brand-name requests are automatically switched to generics unless medically justified.
You have the right to ask for the brand-name version. But if you do, you’ll likely pay more-sometimes a lot more. And your insurer might make you pay the full price out of pocket.
What Should You Do?
Ask your doctor: “Is there a generic for this?” If yes, ask your pharmacist: “Can I get the generic?” Don’t assume the brand is better. The data doesn’t support it.
If you’ve been on a brand-name drug for years and feel fine, there’s no need to switch. But if you’re paying hundreds a month and the generic is available, ask. It’s your right.
And if you switch and feel different? Don’t ignore it. Track your symptoms. Talk to your pharmacist. They can help you figure out if it’s the inactive ingredients-or if it’s something else.
Generics aren’t second-rate. They’re science-backed, cost-effective, and just as safe. For 90% of prescriptions in the U.S., they’re the smart choice. And for millions of people, they’re the only choice that keeps them alive and healthy.
How to Check If Your Drug Has a Generic
You can look up your drug on the FDA’s Drugs@FDA database. Search by brand name. If it says “Therapeutic Equivalence Code: A,” it means the generic is approved as equivalent. If it says “B,” it’s not considered interchangeable.
Or use GoodRx. Just type in your drug. It shows you the brand price and every generic option, with prices from local pharmacies.
It’s simple. And it can save you hundreds-or thousands-each year.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they deliver the same amount of medicine into your bloodstream at the same rate. Large studies involving millions of patients confirm that generics work just as well for conditions like high blood pressure, diabetes, depression, and epilepsy.
Why do generic pills look different from brand-name pills?
Brand-name drug manufacturers hold trademarks on the appearance of their pills-color, shape, size, and markings. Generic manufacturers can’t copy those designs, so they make their own versions. These differences are only cosmetic. They don’t affect how the drug works. The active ingredient is identical.
Can inactive ingredients in generics cause side effects?
Yes, but it’s rare. Inactive ingredients like dyes, fillers, or preservatives can cause reactions in people with allergies or sensitivities. For example, someone allergic to lactose might react to a generic that uses it as a filler. These cases make up less than 0.1% of all generic switches. If you notice new side effects after switching, talk to your pharmacist. They can check the ingredients and suggest another generic version if available.
Are all generics made in the U.S.?
No. Many generics are made in countries like India and China. But the FDA inspects all manufacturing facilities-domestic and foreign-with the same strict standards. Over 3,500 inspections are done each year. Less than 0.5% of facilities have been flagged for quality issues in recent years. The FDA pulls unsafe products immediately.
Should I avoid generics for heart or thyroid medications?
Not necessarily. For drugs like warfarin, levothyroxine, or phenytoin-called narrow therapeutic index (NTI) drugs-the difference between an effective dose and a harmful one is small. Some doctors prefer to keep patients on one version to avoid tiny fluctuations. But the FDA still requires these generics to meet the same bioequivalence standards. Studies show they’re safe and effective. If you’re stable on a brand-name version, stick with it. If you switch, monitor your symptoms and get blood tests as advised by your doctor.
Luke Davidson
January 22, 2026 AT 16:56My pharmacist even showed me the FDA equivalence code. It’s wild how much we’re overpaying out of habit.
Karen Conlin
January 23, 2026 AT 18:11Stop letting marketing scare you. The FDA doesn’t lie. And if your doctor says ‘stick with brand,’ ask them if they’re getting kickbacks.
asa MNG
January 23, 2026 AT 20:51then i switched back to zoloft and boom - peace. so maybe it's not always the same? idk man just saying...
Sushrita Chakraborty
January 24, 2026 AT 16:25Josh McEvoy
January 25, 2026 AT 04:04turned out i just forgot to take it for 3 days. then i took the generic and my bp was better than ever. weird.
Heather McCubbin
January 26, 2026 AT 21:00Sawyer Vitela
January 27, 2026 AT 08:56Shanta Blank
January 28, 2026 AT 12:08Tiffany Wagner
January 28, 2026 AT 12:45Chloe Hadland
January 30, 2026 AT 06:05Amelia Williams
January 31, 2026 AT 14:40Viola Li
February 1, 2026 AT 23:40Dolores Rider
February 2, 2026 AT 20:10